A new generation of API-based interoperability standards is emerging. In contrast to traditional interface specifications, these new approaches focus on reuse of standardized APIs and other “building blocks” which can often be re-combined to address new high-level use-cases without requiring a “start from scratch” for each new use-case.
API access to Health IT systems is not new, but following the JASON report and the JASON Task Force recommendations to the HIT Standards and Policy Committees, there is growing interest into a standards-based API that could become widely supported across many kinds of Health IT. One particular emerging standard, HL7’s Fast Healthcare Interoperability Resources (FHIR) shows promise as becoming a widely supported standard. Vendors and some large provider groups have created the Argonaut Project to define and publish implementation guides in an effort to standardize FHIR implementations across the Health IT community. The FHIR standard specifies many low-level data access services that can be used as “building blocks” to assemble more complex interoperability functionality.
API-based approaches to interoperability have the advantage that APIs can be assembled to rapidly create different kinds of aggregate functions. However, API-based interoperability still requires attention to important implementation details, similar to traditional interoperability specifications. In particular, given the flexibility of APIs, an API-based approach will need to address many required and optional constraints that are necessary to support a desired use-case. For example, if using FHIR as the base API specification, here are some of the constraints that should be considered:
- Which specific data resources are required for the intended interoperability use-case (e.g., patient, encounter, observation)?
- For each resource, what constraints are placed on the values that are allowed for the resource’s data elements (e.g., LOINC, SNOMED)?
- What transport will be used to move the resources back and forth (e.g., HTTP, batch files)?
- Which API operations (e.g. GET (read), PUT (write)) are required?
- For each operation, what operational parameters are required (e.g., supported query parameters for GET)?
- What security model is used to handle authentication, authorization, and encryption (e.g., OAuth, TLS)?
- What other standards are necessary for the overall use-case to be deployed (e.g., HTML, JSON, etc.)?
A specific API-based interoperability use-case will probably need to specify, in the form of an implementation specification, most of the above categories. Some API standards, such as FHIR, contain formal mechanisms (Profiles, Conformance Statements) for specifying constraints, though even a comprehensive specification like FHIR will require that some of the constraints are documented outside of the standard’s formal tools.
To give a more concrete example, consider the “SMART on FHIR” interoperability specification. SMART on FHIR defines a mechanism for interoperable “SMART Apps” that can be plugged in to EHRs and other Health IT systems. Each SMART App can expose a user interaction, and can access data in the underlying system. This presents a powerful way to extend EHR capabilities via “pluggable” app functionality. Dozens of SMART apps are available, with more expected in the future. These apps serve many different clinical needs, yet they all use the same underlying FHIR-based API functionality. However, even though SMART apps are all based on the FHIR standard, it’s not sufficient to simply say “use FHIR”. Here are some of the additional specifications that are needed:
- Resources – Which FHIR resources are available to the App developer? Many EHR vendors are choosing to expose some of the resources defined in ONC’s 2015 Edition Health IT Certification Criteria API requirement. Typical resources available include: Patient, Encounter, Condition, Observation, etc. Not all vendors will elect to expose the exact same set of resources, and some apps may require resources that are not contained in the 2015 Certification list, such as Schedule.
- Resource Profiles – For each supported resource, the FHIR implementation will follow some Profile that specifies how the data fields in the resource will be populated. The Profile will usually define the cardinality of the data (zero, one, or many instances allowed) as well as the Value Sets supported (e.g., LOINC, SNOMED, RxNorm, etc.) Note that formal use of FHIR Profiles is not widely supported at present, so the data constraints are often documented via spreadsheet or other informal means.
- Transport – SMART Apps use HTTP as the transport since they are designed to be interactive and need real-time access to EHR data. The FHIR specification contains a clear mapping of standard data operations (read, write, update, etc.) to the standard HTTP verbs (PUT, GET, etc.)
- API Operations – The 2015 Certification specification currently requires that EHRs support “read only” operations, using the HTTP GET operation. Some vendors have begun to support selected “write” operations using POST, PUT, or UPDATE. Note that the supported write operations may apply only to certain resources. For example, an app might be able to PUT a new Observation, but not be allowed to PUT a new Encounter.
- Parameters – for each resource and operation, the interoperability specification will need to specify which data access parameters are supported. Typically, these include the types of query functions supported by the GET operation. For example, some implementation will support “GET Patient” using the patient’s medical record number, but might not support a “GET Patient” using the SSN or a hospital room number.
- Security Model – The SMART on FHIR specification makes heavy use of the OAuth 2 security standard to orchestrate the HTTP transactions. OAuth may be combined with OpenID Connect in order to cover both authentication and authorization. HTTPS (TLS) is required for on-the-wire encryption. Note that the OAuth 2 standard (which is managed by the IETF) requires its own implementation guide to constrain it for healthcare uses.
- Other Standards – SMART Apps can use HTML5 to control the visual expression of the app, so in some sense, HTML5 is part of the overall specification for SMART on FHIR.
- Trust Relationship – For interoperability using FHIR to work, a trust relationship must be established between entities (ie an EHR/clinical system and an app). This is currently being accomplished by establishing siloed ecosystems. Without an established trust relationship, access to information is not possible regardless of the standards used.
This example illustrates that even though API-based interoperability enables powerful new approaches, there is still a need to carefully specify and constrain each layer of the overall interface orchestration in order to achieve the desired degree of standardization and interoperability.
Text developed by the Health IT Standards Committee as part of the 2017 ISA Task Force
NCPDP Connectivity Operating Rules Implementation Guide an API Application Programming
NCPDP Connectivity Operating Rules Implementation Guide - “An API – application programming interface – at its most basic level, allows your product or service to talk to other products or services. In this way, an API allows you to open up data and functionality to other developers and to other businesses. It is increasingly the way in which agencies and companies exchange data and services, both internally and externally”. There are common technical and practical choices companies need to be aware of when using APIs. This document lays out some of the requirements to ensure the NCPDP Standards employ the API standards appropriately.
For details, refer to the Connectivity Operating Rules Implementation Guide at NCPDP Standards (https://standards.ncpdp.org/Access-to-Standards.aspx).
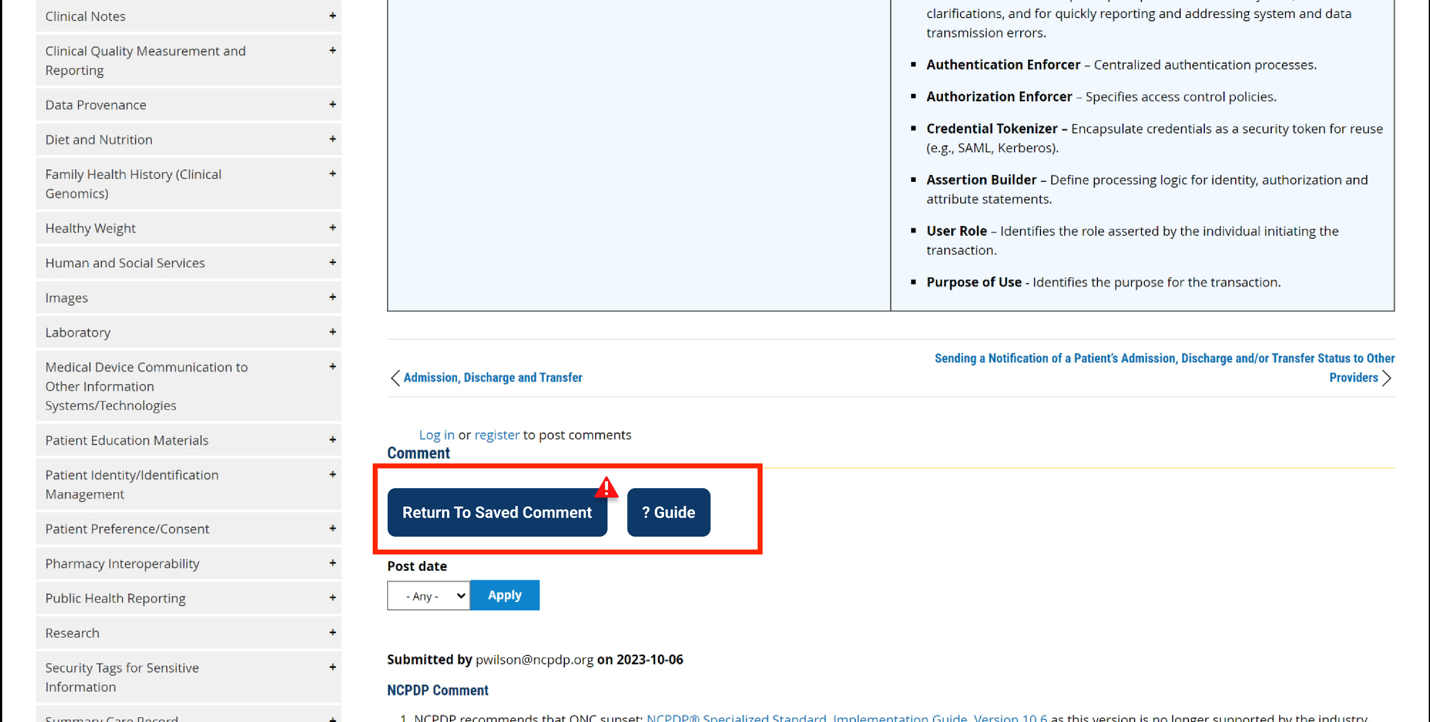
Comment
Submitted by reinaldovel on
Register for course Understanding Emerging API-Based Standards
How do I register for this course: Understanding Emerging API-Based Standards
Submitted by Brett Andriesen ![]() on
on
This is not a course, just…
This is not a course, just an educational description of API standards.
Submitted by mattreid on
Patient Privacy
The AMA wholeheartedly supports the right of patients to receive their medical information using smartphone applications (apps), but is concerned about the lack of safeguards to ensure that patients understand what they are consenting to when they grant permission to an app to access their information. These apps share sensitive health information with third parties, often without an individual's knowledge. Much of this information can end up in the hands of data brokers and be used or sold for advertising and marketing. Data being used in this way may ultimately erode patients’ privacy and their willingness to disclose information to their physicians.
As a first step to address this issue, the AMA is calling for controls to be instituted that establish transparency as to how health information is being used, who is using it, and how to prevent the profiteering of patients’ data. To help provide a minimal amount of transparency to patients about how a health app will use their health information, the federal movement should implement a basic privacy framework requiring certified EHR vendor APIs to check an app’s “yes/no” attestations to:
- Industry-recognized development guidance
- Transparency statements and best practices
- A clear privacy notice to patients


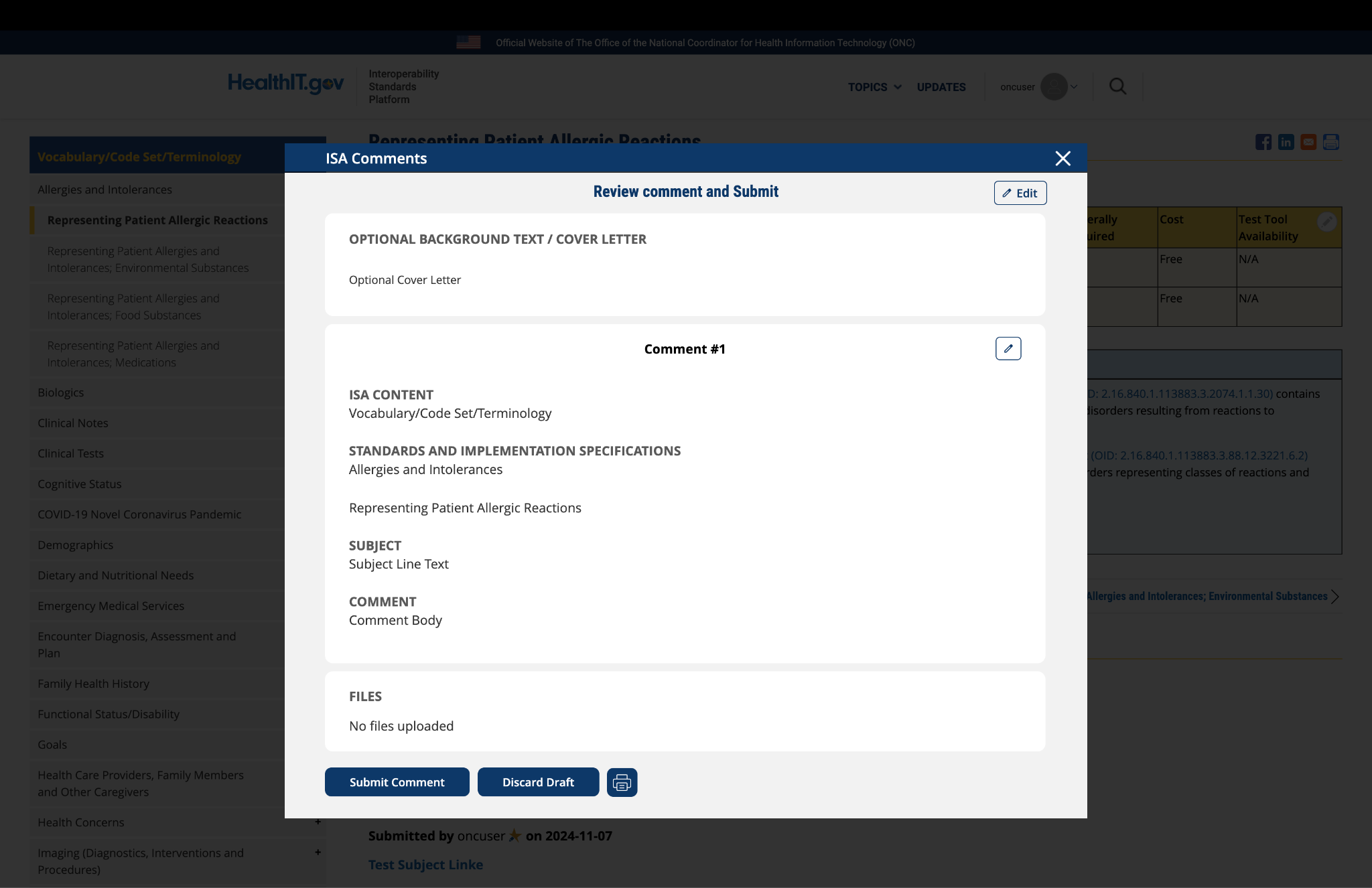
Submitted by pwilson@ncpdp.org on
NCPDP Comments
For details, refer to the Connectivity Operating Rules Implementation Guide at NCPDP Standards .