| Type | Standard / Implementation Specification | Standards Process Maturity | Implementation Maturity | Adoption Level | Federally required | Cost | Test Tool Availability |
|---|---|---|---|---|---|---|---|
|
Standard for observations
|
Final
|
Production
|
No
|
Free
|
N/A
|
||
|
Standard for observation values
|
Final
|
Production
|
No
|
Free
|
N/A
|
||
|
Emerging Implementation Specification
|
In Development
|
Feedback requested
|
Feedback Requested |
No
|
Free
|
| Limitations, Dependencies, and Preconditions for Consideration |
Applicable Value Set(s) and Starter Set(s)
|
|---|---|
|
|
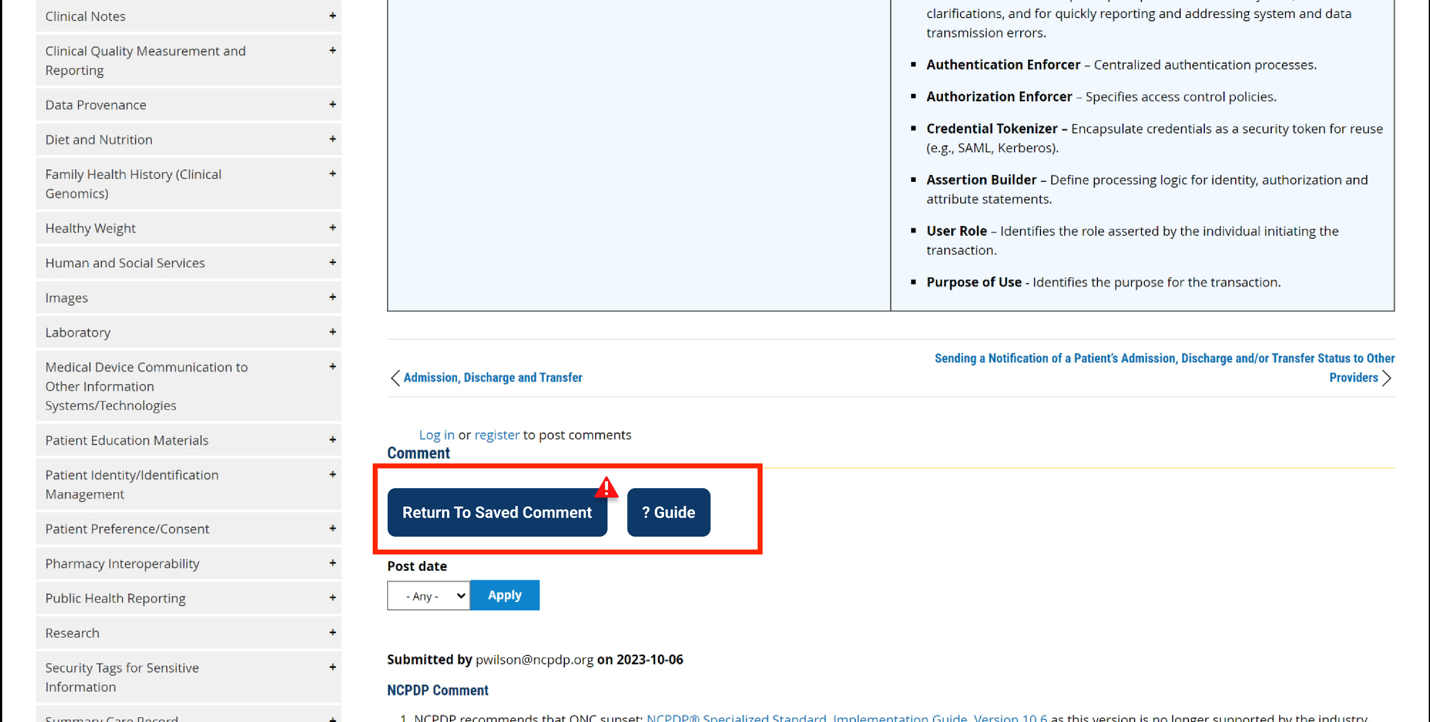
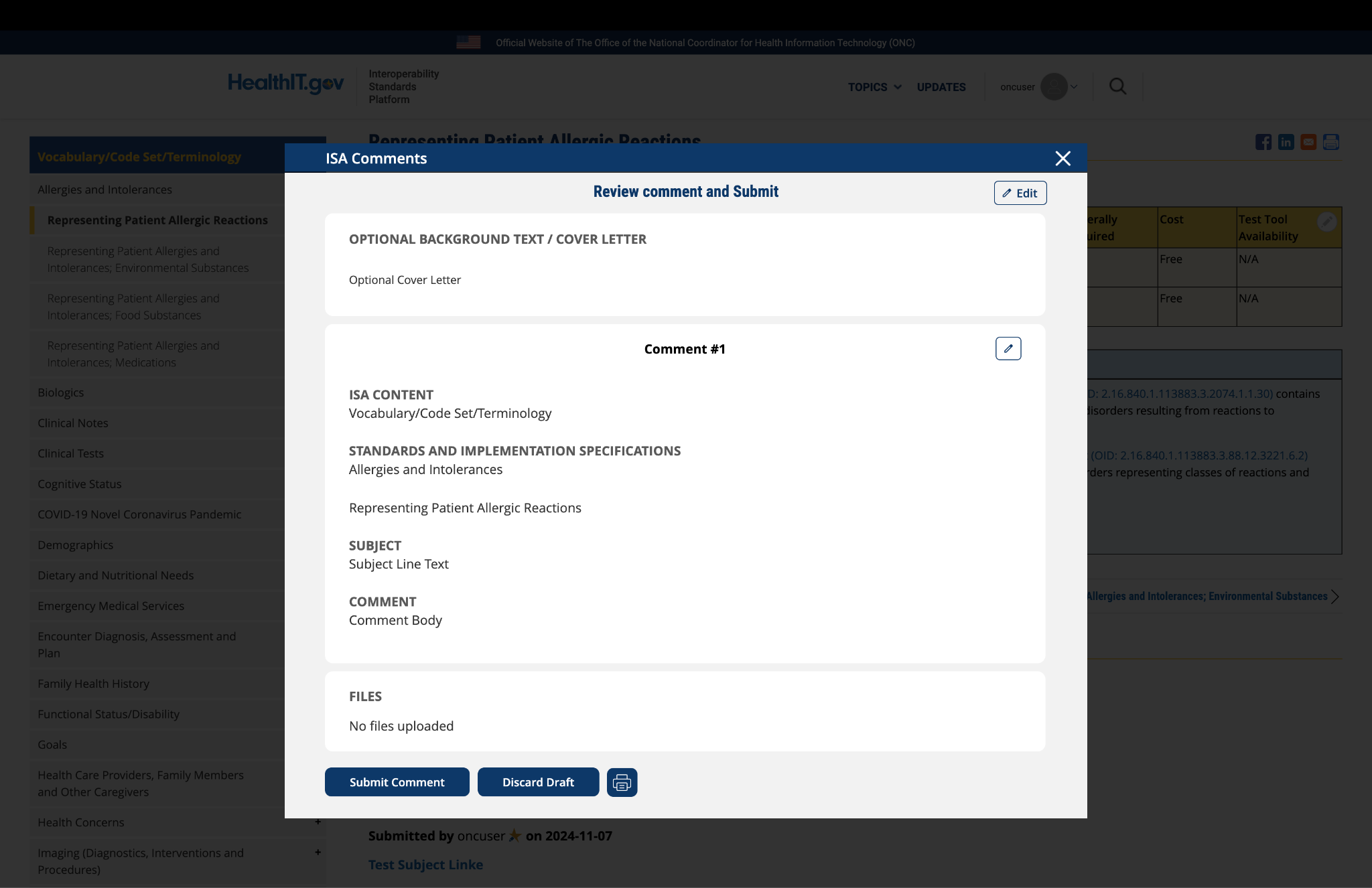
Comment
Submitted by gldickinson on
Preserving Clinical Context
General Comments:
USCDI specifies lots of clinical data classes and data elements
- Resolving to myriad de-coupled fragments
- With vanishingly little focus on:
- Clinical context and vital inter-relationships, e.g., between problems, diagnoses, complaints, symptoms, encounters, history and physical findings, allergies, medications, vaccinations, assessments, clinical decisions, orders, results, diagnostic procedures, interventions, observations, treatments/therapies, referrals, consults, protocols, care plans and status...
- Elements and context + purpose of capture: e.g., blood pressure, its measurement (systolic, diastolic), its unit of measure (mm/Hg), its reason for capture, its context of capture (sampling site, sampling method, patient position, at rest/during/post exercise...
It is crucial to consider and determine/resolve how clinical content and context are bound together and preserved in USCDI. The ultimate end user (often a clinician) must be able to readily discern context and inter-relationships – otherwise USCDI places an undue (and often unresolvable) burden on this user. Only the source EHR/HIT system can structure clinical content and context properly. Once data is stuffed into the USCDI framework and related exchange artifact (e.g., FHIR resources) this opportunity is forever lost.
Submitted by mattreid on
The AMA requests that the…
The AMA requests that the Current Procedural Terminology (CPT) code set be added to the standards listed in Section I: Representing Patient Functional Status and/or Disability. CPT codes 99455 and 99456 identify the completion of medical history, examination, diagnosis, development of a treatment plan, and completion of necessary documents for a patient with a work related or medical disability.
Functional status and disability are also identified in the Physical Therapy Evaluations codes, 97161 – 97164, and Occupational Therapy Evaluations codes, 97165 – 97167, which include patient history, examination, clinical decision making, and development of a treatment plan.
CPT is a comprehensive and regularly curated uniform language that accurately describes medical, surgical, and diagnostic services and provides for reliable communication among users. It has an extremely robust and mature development process with open and transparent meetings and clinical input from national medical specialties and relevant stakeholders. It is the most widely adopted outpatient procedure code set. Use of the CPT code set is federally required under HIPAA.
Submitted by cmcdonald on
The use of OIDs alone is a…
The use of OIDs alone is a bad way to suggest a value set. Readers need some way to see the actual content of the value set, either via URL or, if it is short, as an actual enumeration.
Submitted by cmcdonald on
The adoption level is…
The adoption level is greatly exaggerated. Only IRFPAI of the CMS assessments provides SNOMED CT options in addition to LOINC LA answer lists. All of the categorical answers have LA codes of which there are about 100 unique codes. Some of the answers also have SNOMED CT codes (about 50 unique such codes). The names of the SNOMED Codes are often approximates of the CMS string name for the codes. All of the other CMS assessments include LOINC LA codes or all of their categorical answers and very few SNOMED CT codes except for yes/no. See https://del.cms.gov/DELWeb/pubDownloadHitCodesForm to verify.
Submitted by dvreeman on
Regenstrief - Comment
It would be worthwhile to clarify what the ISA means by functional status and/or disability. These words mean different things to different audiences. We recommend anchoring the ISA notion to the WHO-developed ICF conceptual framework for describing functioning and disability. The ICF has a biopsychosocial model of disability, based on an integration of the social and medical models of disability.
In this model, functioning is an umbrella term for body function, body structures, activities and participation. It denotes the positive or neutral aspects of the interaction between a person’s health condition(s) and that individual’s contextual factors (environmental and personal factors).
Disability is an umbrella term for impairments, activity limitations and participation restrictions. It denotes the negative aspects of the interaction between a person’s health condition(s) and that individual’s contextual factors (environmental and personal factors).
So, what we believe the ISA to be referring to in this interoperability need is the “middle” part of the ICF: the activities of people (functioning at the level of the individual) and the activity limitations they experience; plus the participation or involvement of people in all areas of life, and the participation restrictions they experience (functioning of a person as a member of society). Such clarifications are important for knowing whether something like “cognitive function” is in or out of this domain.
We propose that it would exclude the notion of functioning at the level of the body, that is, impairments of body functions and structures (e.g. measurement of deep tendon reflex of biceps). It would also exclude the notion of environmental factors (e.g. physical geography), whether facilitators or barriers, that affect a person’s experiences.
With that as the framing, we concur with the identification of the terminologies listed in this domain (LOINC and SNOMED CT) as the most appropriate for the observations and observation values related to functioning. In post-acute care settings, functional status is a required component (e.g. Section GG) of the CMS assessment instruments (e.g. MDS, LCDS, IRF-PAI, and OASIS). Through close collaboration between CMS and Regenstrief, all of the variables in these instruments are represented in LOINC. There are other sets of relevant patient reported variables (such as the PROMIS physical function short form, Hip Dysfunction and Osteoarthritis Outcome Score, etc) and clinical assessments of function represented in LOINC. The American Physical Therapy Association identified all of the variables for its national outcomes registry (including items related to functioning) with LOINC.
It is worth noting that LOINC represents the strings of the observation values for standardized assessments as LOINC Answer codes, but these answers for many standardized assessments of functioning are not well represented in SNOMED CT due to their specialized nature. So, just like standardized nursing assessments, LOINC Answer codes should be used to reflect the precise responses on these functional status assessments. The “Adoption Level” for SNOMED CT in this context should be one star at best. There are very few functional status observation values that are even represented in SNOMED CT, and their deployment in this context is very limited.
Last, the NMMDS reference in “Applicable Value Set(s) and Starter Set(s)” should be removed because the NMMDS is about administrative and management information for the provision of nursing care. It doesn’t have variables related to an individual’s functioning/disability.
Submitted by mattreid on
AMA's comments to ONC on proposed 2018 ISA
On behalf of American Medical Association (AMA) I appreciate the ability to comment on the 2018 Interoperability Standards Advisory (ISA).
Comment:
The AMA recommends adding the “Guides to the Evaluation of Permanent Impairment, Sixth Edition” (“Guides”) as an additional resource for this interoperability need in the Limitations, Dependencies, and Preconditions for Consideration. The Guides are a standardized, objective approach to conducting impairment ratings that result in detailed documentation of functional outcomes, physical findings, and clinical test results and have been shown to improve the overall consistency, transparency, and precision of impairment ratings. Users include physicians, other health care providers, attorneys, employers, and claims professionals. The Guides are adopted by U.S. Department of Labor’s Division of Federal Employees’ Compensation for schedule award entitlement determinations. They are also adopted in 19 states and used internationally in Canada, Australia, New Zealand, Hong Kong, Korea, South Africa, and The Netherlands.
Submitted by dvreeman on
The standards named in this…
The standards named in this domain (LOINC and SNOMED CT) are appropriate and we concur with their inclusion here. However, a couple of clarifications are needed. The first bullet should be removed as it suggests that the CMS-required MDS should be used more widely and in different settings than for which it is designed. The IMPACT Act requires that CMS make certain assessment data elements standardized and interoperable so that this data may be exchanged and used by post-acute care and other providers to support care coordination and improved outcomes. CMS is working directly with the Regenstrief Institute to represent all data elements in the assessment instruments they require in different care settings (e.g. MDS, LCDS, IRF-PAI, and OASIS) in LOINC. This work includes current versions of these instruments, as well as their intended harmonization over time.
In addition, many clinical assessments of functional status are well represented in LOINC and SNOMED CT.
Submitted by kwboone on
None of the three existing…
None of the three existing CMS assessment tools for functional status assessment (MDS, OASIS, IRF-PAI) adequately covers all patients. We need a uniform assessment instrument.


Submitted by ragnhildurb on
Comments from the Alliance for Nursing Informatics
Thank you for the opportunity to provide comments on the Interoperability Standards Advisory (ISA) and the Standards Version Advancement Process (SVAP). The ANI strongly supports further development to include Functional Status standards in regulations and as federal program requirements.
Please see attachment for our full comments
ANI COMMENTS on ISA-SVAP _FINAL.pdf