
An official website of the United States government
Here’s how you know
Official websites use .gov
A
.gov
website belongs to an official government organization in the
United States.
Secure .gov websites use HTTPS
A
lock
(
) or
https://
means you’ve safely connected to the .gov website. Share sensitive
information only on official, secure websites.
State of Interoperability among U.S. Non-federal Acute Care Hospitals in 2018
No. 51 | March 2020
Achieving nationwide interoperability is a stated objective of the federal government. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ( 1) and the 21st Century Cures Act of 2016 (2) call for specific actions to improve the seamless sharing of data across the care c ontinuum. Efforts are also underway to consolidate the number of methods used to exchange patients’ health information. In this data brief, we report the state of interoperability among non -federal acute care hospitals . We examine methods hospitals use to exchange and query for electronic health information. Additionally, we report on barriers to interoperability as well as the extent to which hospitals participate in health information exchange organizations (HIOs).
Highlights
- Almost half of hospitals engaged in all four domains of interoperability (send, receive, find, integrate)
- Electronic availability of patient health information from outsides sources increased by 10 percent in 2018 resulting in over half of hospitals having electronic patient health information available at the point of care.
- On average, hospitals used about three different electronic methods to electronically exchange summary of care records with outside providers.
- Small, rural, and critical access hospitals (CAHs) were less likely to participate in national networks and state, regional, or local HIOs than their counterparts.
The percent of hospitals with the capability to integrate data into their electronic health record (EHR) increased by 17 percent between 2017 and 2018.
Figure 1: Percent of U.S. non-federal acute care hospitals that electronically find patient health information, and send, receive, and integrate patient summary of care records from sources outside their health system, 2014-2018.
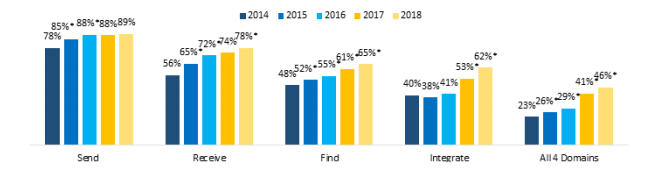
Notes: *Significantly different from previous year (p<0.05).
- Almost half of hospitals engaged in all four domains of interoperability (e.g., send, receive, find, integrate).
- The percentage of hospitals that electronically received and searched for or queried summary of care records increased in 2018 compared to 2017.
The percent of hospitals reported that their providers have necessary information electronically available from outside sources increased between 2017 and 2018.
Figure 2: Percent of U.S. non-federal acute care hospitals whose providers have necessary patient information electronically available from outside providers or sources, 2015-2018.
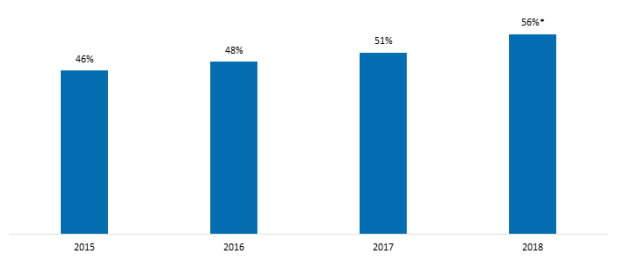
Notes: *Significantly different from prior year (p<0.05).
- Over half of hospitals reported having necessary information electronically available in 2018.
- During 2015-2017, there was not a significant change in the percentage of hospitals having necessary information electronically available from outside sources.
The percent of hospitals that often or sometimes used patient health information electronically received from outside sources significantly increased in 2017 and 2018.
Figure 3: Percent of U.S. non-federal acute care hospitals’ that often or sometimes use patient health information received electronically from providers or sources outside their health system when treating patients, 2015-2018
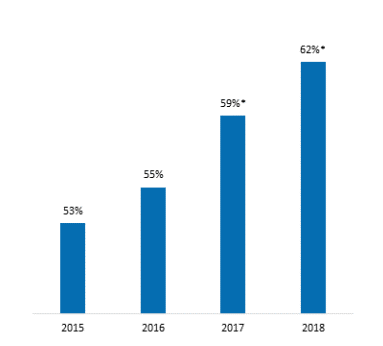
Table 1: Reasons for rarely or never using patient health information received electronically from providers or sources outside their health system when treating patients, 2018.
| Reason for not Using Patient Health Information | Percent |
|---|---|
| Information not always available when needed (e.g. not timely) | 52% |
| Information is available but not integrated into EHR | 50% |
| Information not presented in a useful format (e.g. too much information, redundant, or unnecessary information) | 34% |
| Information that is specific and relevant is hard to find | 23% |
| Information available and integrated into EHR but not part of clinicians’ workflow | 17% |
| Do not trust accuracy of information | 10% |
| Vocabulary and/or semantic representation differences limit use | 6% |
| Other | 17% |
Notes: *Significantly different from prior year (p<0.05).
- During 2015-2018 the percent of hospitals that reported often or sometimes using patient health information increased by 17 percent.
- About six in 10 hospitals reported often or sometimes using patient health information they electronically receive.
- The top reasons cited for not using patient health information electronically received from outside sources were information was not always available and the data were not integrated into the EHR.
- Among hospitals that rarely or never used electronically received information, one-third reported that information was not presented in a useful format and one-fifth indicated that information was difficult to find.
- Less than 10 percent of hospitals reported that vocabulary and/or semantic representation differences limited the use of patient health information.
The most frequently reported barrier to electronic exchange was difficulty exchanging data across different EHR vendor platforms.
Table 2: Percent of U.S. non-federal acute care hospitals that experienced barriers when trying to electronically send, receive, or find health information to/from other care settings or organizations, 2018.
| Percent | |
|---|---|
| Barriers related to electronically sending patient health information Percent | |
| Difficult to find providers’ addresses | 60% |
| Exchange partners’ EHR system lacks capability to receive data | 54% |
| Exchange partners’ we would like to send data to do not have an EHR or other electronic system to receive data | 52% |
| Many recipients of care summaries report that the information is not useful | 46% |
| Cumbersome workflow to send the information from our EHR system | 32% |
| The complexity of state and federal privacy and security regulations makes it difficult for us to determine whether it is permissible to electronically exchange patient health information | 23% |
| Lacking the technical capability to electronically send patient health information to outside providers or other sources | 12% |
| Barriers related to electronically receiving patient health information | |
| There are providers whom we share patients with that don’t typically exchange patient data with us | 65% |
| Difficult to match or identify the correct patient between systems | 54% |
| We lack the technical capability to electronically receive patient health information from outside providers or other sources | 23% |
| Other barriers related to exchanging patient health information | 78% |
| Greater challenges exchanging data across different vendor platforms | |
| Paying additional costs to exchange with organizations outside our system | 43% |
| Develop customized interfaces in order to electronically exchange health information | 39% |
- Over 60 percent of hospitals reported difficulty finding providers’ addresses.
- Over half of hospitals reported difficulty to match or identify correct patient between systems.
- Half of hospitals indicate their exchange partners lack the capability to receive data, either because their EHR system lacks the capability or because their exchange partners lack a system to electronically receive the data.
- Almost half of hospitals reported that summary of care records were not considered useful by recipients.
- About four in 10 hospitals cited barriers related to costs, including developing customized interfaces in order to electronically exchange health information and paying additional costs to exchange data with outside providers.
- Lacking the technical capability to electronically send patient health information was the least cited barrier to electronically exchanging patient health information.
A majority of hospitals reported using a mix of electronic and non-electronic methods for exchanging summary of care records.
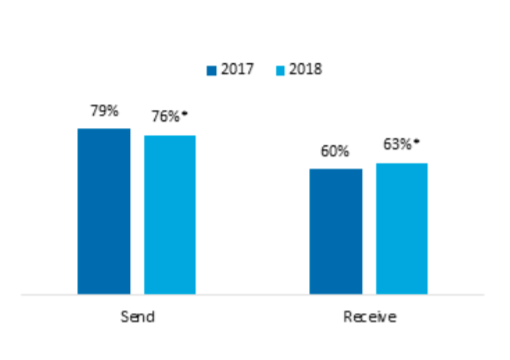
Figure 4: Percent of U.S. non-federal acute care hospitals that often or sometimes receive/send summary of care records by method type, 2017- 2018.

Notes: *Significantly different from a corresponding category in previous year (p<0.05).
- In 2018, three-quarters of hospitals used mixed methods to send summary of care records and two-thirds used mixed methods to receive summary of care records.
- About one in 10 hospitals used electronic only methods for sending and receiving summary of care records.
- In 2018, almost one in five hospitals relied on non-electronic methods to receive summary of care records
The majority of hospitals used more than one electronic method to electronically exchange summary of care records with outside providers.
Figure 5: Average number of electronic methods hospitals use to exchange health information, 2017-2018.
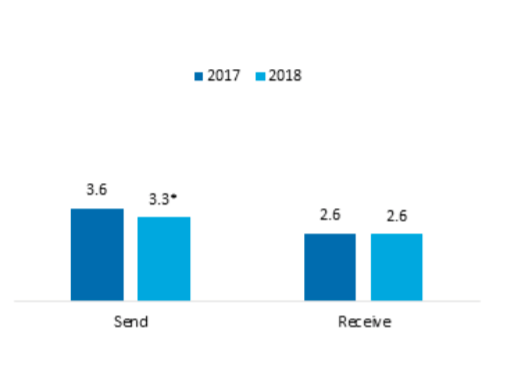
Figure 6: Percent of hospitals using more than one electronic method to exchange health information, 2017- 2018.
Notes: *Significantly different from a corresponding category in previous year (p<0.05).
- On average, hospitals used about three different electronic methods for sending (3.3) and receiving (2.6) summary of care records in 2018.
- The average number of electronic methods used for sending summary of care records declined between 2017 and 2018.
- In 2018, almost one in five hospitals relied on non-electronic methods to receive summary of care records
- The proportion of hospitals using more than one electronic method for receiving summary of care records increased by three percentage points between 2017 and 2018.
The percent of hospitals that used mail or fax for sending and receiving summary of care records increased in 2018.
Table 3: Percent of U.S. non-federal acute care hospitals that often or sometimes send or receive summary of care records with sources outside their hospital system by method, 2017-2018.
| Send | Receive | |||
|---|---|---|---|---|
| Methods | 2017 | 2018 | 2017 | 2018 |
| Method Not Using a Third-Party | ||||
| Mail or fax | 66% | 71%* | 73% | 76%* |
| eFax using EHR | 63% | 66% | 45% | 52%* |
| Provider portal for view only access to EHR system | 58% | 49%* | 39% | 37% |
| Interface connection between EHR systems (e.g. HL7 interface) | 49% | 42%* | 31% | 30% |
| Direct access to EHRs (via remote or terminal access) | 49% | 37%* | 30% | 26%* |
| Method Using a Third-Party | ||||
| Standalone Health Information Service Provider (HISP) or HISP provided by a third party (e.g. DIRECT) | 68% | 61%* | 49% | 49% |
| State, regional, or local HIO | 55% | 59%* | 43% | 46% |
| Single EHR vendor network | 42% | 43% | 37% | 41%* |
| Multi-EHR vendor network (e.g. CommonWell) | 40% | 35%* | 34% | 32% |
Notes: *Significantly different from previous year (p<0.05).
- About seven in 10 hospitals continued to use mail or fax for sending and receiving summary of care records in 2018.
- About six in 10 hospitals reported using a HISP to send summary of care records. This was the most common electronic method for sending and receiving summary of care records in 2017 and 2018.
- The use of HIO for sending summary of care records and single EHR vendor network for receiving summary of care records significantly increased during 2017-2018.
- The least commonly used method to electronically send or receive summary of care records was direct access to EHRs via a remote or terminal access.
- There were decreases in the percentage of hospitals using stand-alone electronic methods not involving a thirdparty for sending summary of care records.
A state, regional, or local HIO was the most common method used to electronically find or query patient health information from outside sources.
Figure 7: Methods used to electronically search for patients’ health information, 2018
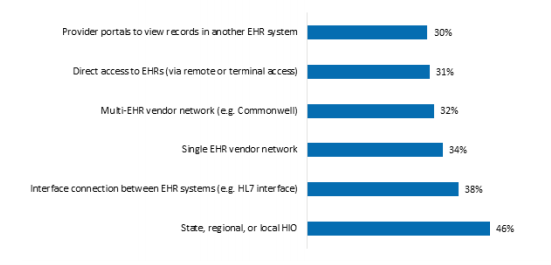
- Almost half of hospitals used state, regional or local HIOs to electronically find or query patient health information from outside sources.
- About one third of hospitals used provider portal, direct access to EHRs, and multi-EHR vendor networks to electronically find patients’ health information.
- On average, hospitals used two methods for finding patients’ health information (not shown in the figure above).
In 2018, about one third of hospitals participated in more than one national health information network (national network).
Table 4: Hospitals’ participation in national networks, 2018.
| Overall National Network Participation | 2018 |
|---|---|
| Percent of Hospitals that Participate in Any Network | 57% |
| Percent of Hospitals that Participate in More than One Network | 33% |
| Average Number of Networks | 1.21 |
| National Network | Percent |
| Single-EHR vendor network | 32% |
| e-Health Exchange | 25% |
| DirectTrust | 21% |
| Sequoia Project’s Carequality | 20% |
| CommonWell Health Alliance | 19% |
| Strategic Health Information Exchange Collaborative (SHIEC)/Patient Centered Data Home (PCDH) | 4% |
- On average, hospitals participated in one national network in 2018
- Single-EHR vendor network is most commonly participated network among hospitals.
- About one-fifth of hospitals participated in CommonWell Health Alliance, DirectTrust, and Carequality, respectively.
Less than half of hospitals participated in both a national network and a state, regional, or local HIO.
Table 5: Percent of U.S. non-federal acute care hospitals that participate in national and state, regional, or local health information networks, 2018.
| Participate in State, Regional, and/or Local HIO | Participate in National Network | |
|---|---|---|
| Yes | No | |
| Yes | 46% | 27% |
| No | 11% | 15% |
- Almost 60 percent of hospitals participated in a state, regional, and/or local HIO.
- A relatively small share of hospitals (15 percent) did not participate in a national network or a state, regional, or local HIO.
Small, rural, and CAHs participated in fewer national and state, regional or local health information networks compared to their counterparts.
Table 6: Percent of U.S. non-federal acute care hospitals that participate in national and state, regional, or local health information networks by hospital type, 2018.
| Type of Network | Medium Large | Small | Suburban Urban | Rural | Non-CAH | CAH |
|---|---|---|---|---|---|---|
| National Network | 64% | 50%* | 64% | 49%* | 60% | 51%* |
| State, regional, or local HIO | 81% | 67%* | 79% | 67%* | 77% | 64%* |
| Both Network Types | 54% | 39%* | 52% | 38%* | 50% | 38%* |
Notes: *Significantly different from a corresponding category presented in the column to the left (p<0.05).
- Less than half of small, rural, and CAHs participated in both national and state, regional, or local health information networks.
- CAHs were the least likely to participate in state, regional, or local HIO (64 percent) compared to non-CAHs (77 percent).
- There was a 14 percentage point difference in the participation in national networks by medium/large hospitals compared to small hospitals.
Summary
Interoperability among U.S. hospitals continues to improve (2). Compared to 2017, hospitals’ rates of engaging in electronically receiving, integrating, and querying data from outside sources increased in 2018. Most hospitals sent (89 percent) and received (78 percent) patient summary of care records from outside sources. Six in ten hospitals were able to find (or query) and integrate patient health information from sources outside their health system. Overall, almost half of hospitals engaged in all four domains of interoperability. These improvements translated to increased availability of information. Over half of hospitals indicated patient health information is electronically available at the point of care, a significant increase over the prior year. Six in 10 hospitals were also using information received electronically from sources outside their health system.
Despite these improvements, a number of barriers are limiting greater progress towards achieving widespread interoperability. Top reasons cited by hospitals for rarely or never using health information received included timeliness of the data and difficulty integrating information into their EHR. Usability issues, such as difficulty locating information and the usefulness of how information is presented, were also cited as barriers to use. However, the most frequently cited barriers to electronically exchanging data were difficulty with cross-vendor exchange, locating provider addresses, and having external providers who don’t typically share data, and matching patients.
In addition to paper-based methods, a majority of hospitals used more than one electronic method for exchanging summary of care records. Hospitals on average were using over three methods to send summary of care records and two different electronic methods to receive this information. The most frequently used electronic methods to send and receive data involved third-parties, such as HISPs and national and regional health information networks. There were decreases in the percentage of hospitals using stand-alone electronic methods that didn’t involve intermediaries. However, about four in 10 hospitals still relied on customized interfaces to exchange information.
National networks that enable exchange across different EHR vendor systems are among the newer methods of exchange. A one third of hospitals were participating in more than one national network. This may reflect that currently hospitals experience difficulties exchanging information with members across different networks. Additionally, almost half of hospitals participated in both national networks and regional, state, local networks. Notably, however, rural, small and CAHs lagged behind their counterparts in the participation in both types of networks to facilitate exchange of health information.
The 21st Century Cures Act called for the creation of a Trusted Exchange Framework and Common Agreement (TEFCA), which would enable providers to exchange data across disparate health information networks (3). The second draft of the TEFCA—which outlines a common set of principles, terms, and conditions to support the development of a Common Agreement—should enable providers to participate in fewer networks and be less reliant on stand-alone, one-off methods of exchange such as interfaces. The newly recognized coordinating entity is taking initial steps to implement the TEFCA (4).
ONC and Centers for Medicare & Medicaid Services (CMS) recently proposed rules intended to reduce barriers identified in this data brief (5,6). For example, ONC proposed a rule for IT developers to meet various conditions for certification, including a requirement not to take any action that constitutes information blocking. ONC and CMS outlined disincentives for health care providers to engage in information blocking (6,7). The CMS also proposed steps to increase the number of providers who submit their digital contact information to the National Plan and Provider Enumeration System, which should reduce problems associated with provider directories reported by hospitals (6). Together, the joint actions of CMS and ONC have potential to improve access and exchange of electronic health information.
Definitions
Non-federal acute care hospital: Hospitals that meet the following criteria: acute care general medical and surgical, children’s general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or state/local government and located within the 50 states and District of Columbia.
Interoperability: The ability of a system to exchange electronic health information with and use electronic health information from other systems without special effort on the part of the user (3). This brief further specifies interoperability as the ability for health systems to electronically send, receive, find, and use health information with other electronic systems outside their organization.
Integrate: Whether the EHR integrates summary of care record received electronically (not eFax) from providers or sources outside your hospital system/organization without the need for manual entry.
Find: Whether providers at your hospital query electronically for patients’ health information (e.g., medications, outside encounters) from sources outside of your organization or hospital system.
Small hospital: Non-federal acute care hospitals of bed sizes of 100 or less.
Rural hospital: Hospitals located in a non-metropolitan statistical area.
Critical Access Hospital: Hospitals with less than 25 beds and at least 35 miles away from another general or critical access hospital.
Health information exchange organization (HIO): State, regional, or local health information network. This does not include local proprietary or enterprise networks.
National network: Health information networks that are nationwide in scope. This includes multi-EHR vendor networks (e.g. Commonwell or e-Health Exchange) which can be used to exchange health information either directly through an EHR or health information exchange (HIE) vendor.
Data Source and Methods
Data are from the American Hospital Association (AHA) Information Technology (IT) Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to measure the adoption and use of health IT in U.S. hospitals. ONC funded the 2018 AHA IT Supplement to track hospital adoption and use of EHRs and the exchange of clinical data.
The chief executive officer of each U.S. hospital was invited to participate in the survey regardless of AHA membership status. The person most knowledgeable about the hospital’s health IT (typically the chief information officer) was requested to provide the information via a mail survey or secure online site. Non-respondents received follow-up mailings and phone calls to encourage response.
The survey was fielded from the beginning of January 2019 to the middle of May 2019. The response rate for non-federal acute care hospitals was 64 percent. A logistic regression model was used to predict the propensity of survey response as a function of hospital characteristics, including size, ownership, teaching status, system membership, and availability of a cardiac intensive care unit, urban status, and region. Hospital-level weights were derived by the inverse of the predicted propensity.
References
1. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), (Pub. L. No. 114 – 10, enacted April 16, 2015), Section 106(b)(1). https://www.gpo.gov/fdsys/pkg/PLAW-114publ10/html/PLAW-114publ10.htm.
2. 21st Century Cures Act, section 4006. https://www.congress.gov/114/statute/STATUTE-130/STATUTE-130-Pg1033.pdf.
3. ONC. Trusted Exchange Framework and Common Agreement (TEFCA). https://healthit.gov/policy/tefca/
4. The Sequoia Project. https://rce.sequoiaproject.org/community-engagement/
5. ONC. Notice of Proposed Rulemaking to Improve the Interoperability of Health Information. https://healthit.gov/wp-content/uploads/2025/07/ONCCuresActNPRM.pdf
6. CMS. Interoperability and Patient Access Proposed Rule. https://www.federalregister.gov/documents/2019/03/04/2019-02200/medicare-and-medicaid-programs-patient-protection-and-affordable-care-act-interoperability-and
7. ONC. Information blocking. https://healthit.gov/information-blocking/
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of Technical Strategy and Analysis, and Talisha Searcy, Director of the Data Analysis Branch.
Suggested Citation
Pylypchuk Y., Johnson C., Patel V. (March 2020). State of Interoperability and Methods Used for Interoperable Exchange among U.S. Non-federal Acute Care Hospitals in 2018. ONC Data Brief, no.51. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix Table A1: Survey questions assessing variation in interoperability among hospitals.
| Question Text | Response Options |
|---|---|
| When a patient transitions to another care setting or organization outside your hospital system, how often does your hospital use the following methods to send a summary of care record? |
Often | Sometimes| Rarely | Never | Don’t Know/NA Methods without intermediaries
|
| When a patient transitions to another care setting or organization outside your hospital system, how often does your hospital use the following methods to receive a summary of care record? |
Often | Sometimes| Rarely |Never | Don’t Know/NA Methods without intermediaries
|
| Do providers at your hospital query electronically for patients’ health information (e.g. medications, outside encounters) from sources outside of your organization or hospital system? |
|
| How often are the following electronic methods used to search for (e.g., query or auto-query) and view patient health information from providers outside your hospital system? |
Often | Sometimes | Rarely | Never | Don’t Know/NA
|
| Does your EHR integrate the information contained in summary of care records received electronically (not eFax) without the need for manual entry? Note: This refers to the ability to add or incorporate the information to the EHR without special effort (this does NOT refer to automatically adding data without provider review). This could be done using software to convert scanned documents into indexed, discrete data that can be integrated into EHR. |
|
| Do providers at your hospital routinely have necessary clinical information available electronically (not e-Fax) from outside providers or sources when treating a patient that was seen by another health care provider/setting? |
|
| How frequently do providers at your hospital use patient health information received electronically (not e-Fax) from outside providers or sources when treating a patient? |
|
| If rarely or never used, please indicate the reason(s) why. Check all that apply. |
|
| Which of the following issues has your hospital experienced when trying to electronically (not eFax) send, receive or find (query) patient information to/from other care settings or organizations? Check all that apply. |
|
| Please indicate whether you have used electronic clinical data from the EHR or other electronic system in your hospital to: (Please check all that apply) |
|
| Which of the following national health information exchange networks does your hospital participate in? |
|
| Please indicate your level of participation in a state, regional, and/or local health information exchange (HIE) or health information organization (HIO). Note: this does not refer to a private, enterprise network. |
|
