
An official website of the United States government
Here’s how you know
Official websites use .gov
A
.gov
website belongs to an official government organization in the
United States.
Secure .gov websites use HTTPS
A
lock
(
) or
https://
means you’ve safely connected to the .gov website. Share sensitive
information only on official, secure websites.
Hospitals Use of Electronic Health Records Data, 2015-2017
No. 46 | April 2019
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 helped to advance the adoption and meaningful use of electronic health records (EHRs). Today, more than 95 percent of hospitals possess an EHR (1). With widespread adoption of EHRs, policy is now shifting towards the use of EHR data. EHR data can improve patient care by giving providers access to evidence based tools that assist with decision making and facilitating clinical practice by automating and streamlining the provider workflow (2). This brief uses data from the American Hospital Association Information Technology Survey to describe trends in the use of EHR data among non-federal acute care hospitals from 2015 to 2017. We defined use of EHR data as a set of ten measures that describe hospital processes for leveraging data within their EHR to inform clinical practice (see appendix for survey details). The data brief also presents variation in the use of this data by hospital characteristics and over time.
Highlights
- As of 2017, 94 percent of hospitals used their EHR data to perform hospital processes that inform clinical practice.
- EHR data is most commonly used by hospitals to support quality improvement (82 percent), monitor patient safety (81 percent), and measure organization performance (77 percent).
- Hospital characteristics significantly impact the use of EHR data – small, rural, critical access, state/local government, and non-teaching hospitals had the lowest rates of using their EHR data.
- A hospital’s use of their EHR data varied significantly by developer.
- Hospitals with the capability to send, find, receive, or integrate external patient data were twice as likely to use their EHR data compared to hospitals that did not engage in these domains of interoperability.
In 2017, 94 percent of hospitals used electronic clinical data from their EHR.
Figure 1: Percent of non-federal acute care hospitals that use their EHR data for at least one of the ten specified measures of hospital processes to inform clinical practice, 2015 – 2017.
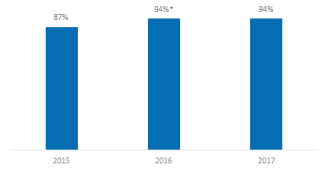
Note: The sample consists of 3,599 non-federal acute care hospitals
- There was a 7 percent increase between 2015 and 2016 in the percent of hospitals that use their EHR data.
Hospitals commonly used their EHR data to support quality improvement (82 percent), monitor patient safety (81 percent), and measure organization performance (77 percent).
Figure 2: Percent of non-federal acute care hospitals that use their EHR data to perform each process that informs clinical practice, 2015-2017.
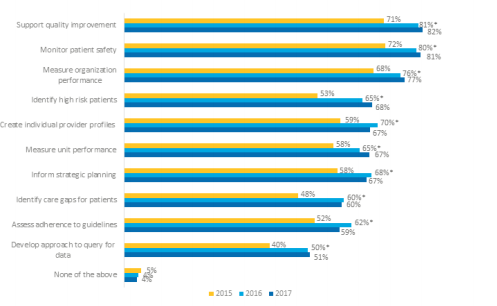
Note: *Significantly higher than the previous year (p<0.05). The sample consists of 3,599 non-federal acute care hospitals.
- There was a significant increase in the use of EHR data between 2015 and 2016 for all measures.
- From 2015 to 2017, the greatest increase in the use of EHR data occurred for identifying high risk patients (15 percent increase), identifying care gaps for patients (12 percent increase), developing an approach to query for patient data (11 percent increase), and supporting quality improvement (11 percent increase).
- The use of EHR data to develop an approach to query for patient data within a hospital network is the least frequent process performed by hospitals from 2015 to 2017 (40 percent, 50 percent, and 51 percent respectively).
- Less than 5 percent of hospitals did not use EHR data from 2015 to 2017 to complete any of the 10 processes.
In 2017, hospitals increased their use of EHR data to perform 7 out of 10 processes, on average.
Figure 3: Average number of EHR data use processes that hospitals engage in to inform clinical practice, 2015-2017.
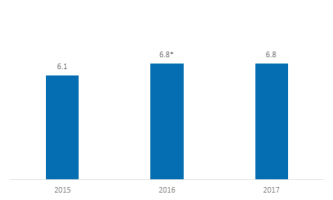
Note: *Significantly different from previous year (p < 0.05). There are 10 measures of EHR data use to inform clinical practice. The sample consists of 3,599 non-federal acute care hospitals. There are 10 measures of EHR data use to inform clinical practice.
- In 2017, hospitals used their EHR data, on average, to perform 7 out of 10 processes.
- Hospitals increased their use of EHR data to inform clinical practice between 2015 and 2016 to an average of seven of ten processes.
- There was a significant increase in the average number of uses for EHR data between 2015 and 2016, but no change between 2016 and 2017.
Small, rural, and critical access hospitals had among the lowest rates of EHR data use to inform clinical practice.
Table 1: Average number of EHR data use processes that hospitals engage in to inform clinical practice by hospital characteristics, 2015-2017.
| 2015 | 2016 | 2017 | |
|---|---|---|---|
| Hospital Size | |||
| Small (less than 100 beds) | 5.2 | 5.8* | 5.7 |
| Medium/ Large (more than 100 beds) | 6.5 | 7.8* | 7.8 |
| Critical Access Hospital | |||
| Yes | 4.8 | 5.3* | 5.2 |
| No | 6.2 | 7.4* | 7.5 |
| Hospital System | |||
| Yes | 6.3 | 7.6* | 7.7 |
| No | 5.1 | 5.4* | 5.1 |
| Geographic Location | |||
| Rural | 5.1 | 5.6* | 5.5 |
| Urban | 6.4 | 7.7* | 7.7 |
| Teaching Status | |||
| Teaching | 6.9 | 7.8* | 7.9 |
| Not Teaching | 5.3 | 6.3* | 6.1 |
| Profit Type | |||
| For Profit | 3.4 | 7.2* | 7.2 |
| Not for Profit | 6.7 | 7.3* | 7.3 |
| State/ Local Government | 5.0 | 5.2 | 5.2 |
Note: *Significantly higher than the previous year (p<0.05). There are 10 measures of EHR data use to inform clinical practice. The sample consists of 3,599 non-federal acute care hospitals. There are 10 measures of EHR data use to inform clinical practice.
- In 2017, medium and large hospitals, hospital systems, urban hospitals, and teaching hospitals had the highest rates of EHR data use to inform clinical practice.
- The greatest increase in the use of EHR data occurred among for-profit hospitals from 3.4 measures in 2015 to 7.2 measures in 2017.
- The smallest changes in the use of EHR data between 2015 and 2017 occurred in small hospitals, hospitals not part of a hospital system, rural hospitals, and state/local government hospitals.
- State and local government hospitals’ use of EHR data did not change between 2015 and 2017.
Hospitals’ use of their EHR data varies by EHR developer.
Table 2: Percent of hospitals by EHR developer that engaged in each of the metrics of EHR data use to inform clinical practice by EHR developer, 2017.
| Allscripts | Cerner | CPSI | Epic | McKesson | MediTech | MedHost | Other | |
|---|---|---|---|---|---|---|---|---|
| Support quality improvement (%) | 74 | 89 | 59 | 96 | 69 | 88 | 65 | 63 |
| Monitor patient safety (%) | 83 | 84 | 69 | 92 | 74 | 87 | 66 | 64 |
| Measure organization performance (%) | 76 | 79 | 51 | 96 | 66 | 83 | 51 | 54 |
| Identify high risk patients (%) | 68 | 78 | 32 | 88 | 52 | 73 | 28 | 40 |
| Create individual provider profiles (%) | 58 | 70 | 36 | 89 | 63 | 69 | 36 | 48 |
| Measure unit performance (%) | 64 | 74 | 29 | 91 | 56 | 68 | 37 | 39 |
| Inform strategic planning (%) | 68 | 71 | 43 | 76 | 61 | 77 | 53 | 39 |
| Identify care gaps for patients (%) | 60 | 63 | 22 | 86 | 41 | 61 | 24 | 36 |
| Assess adherence to guidelines (%) | 49 | 59 | 28 | 82 | 50 | 63 | 26 | 35 |
| Develop approach to query for data (%) | 51 | 47 | 15 | 82 | 27 | 52 | 18 | 26 |
| None of the above (%) | 2 | 2 | 10 | 0 | 4 | 2 | 11 | 20 |
| Total Hospitals (N) | 105 | 587 | 257 | 857 | 102 | 540 | 69 | 103 |
Note: The sample consists of 3,599 non-federal acute care hospitals. “Other developer” encompasses all hospitals that reported using an EHR, but did not use one of the developers mentioned in the table. Examples include: athenahealth, eClinical works, GE, HMS, Health Care System, MED3000, MedWorx, Nextgen, Prognosis, QuadraMed, Sage, Siemens, self- developed, or Vitera/ Greenway.
- The EHR developers with the highest use of their data to inform clinical practice include Epic, Meditech, and Cerner.
- In 2017, the most used aspect of EHR data for hospitals with Cerner (89 Percent), Epic (96 percent), and MediTech (88 percent) was to support quality improvement.
- Most hospitals that used CPSI (69 percent), McKesson (74 percent), MedHost (66 percent), or other EHR developers (64 percent) used their data to monitor patient safety.
- Hospitals with any developer, except Epic and Allscripts, were least likely to use their data to develop an approach to query for patient data. Hospitals using Epic were least likely to use their EHR data to inform strategic planning and hospitals with Allscripts were least likely to use their EHR data to assess adhere to guidelines.
- Hospitals using CPSI, Medhost, or one of the unspecified EHR developers were more likely to report that they did not use their EHR data.
Hospitals that engaged in the four domains of interoperability used their EHR data in substantially more ways than hospitals that could not engage in the four domains of interoperability.
Figure 4: Average number of EHR data use processes that hospitals engage in to inform clinical practice by hospital interoperability status, 2017.
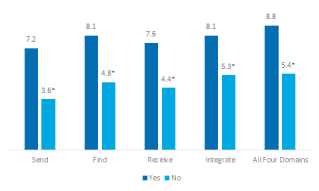
Note: *Significantly lower than hospitals that were interoperable for the respective measure (p<0.05). The sample consists of 3,599 non-federal acute care hospitals. There are 10 measures of EHR data use to inform clinical practice.
- Hospitals engaged in an interoperability domain (i.e., send, find, receive or integrate) used their EHR data for least 7 processes, compared to 4 processes for hospitals that did not engage in an interoperability domain.
- Hospitals that engaged in all four interoperability domains had the highest rates of EHR data use, on average 8.8 processes.
- Hospitals without the ability to send patients’ health information to other hospitals outside their organization/system had the lowest use of their EHR data, on average 3.6 processes.
Hospitals participating in CMS Innovation Models had significantly higher rates of EHR data use compared to hospitals that did not participate in these programs.
Figure 5: Average number of EHR data use processes that hospitals engage in to inform clinical practice by participation in Centers for Medicare and Medicaid (CMS) Innovation Models, 2017.
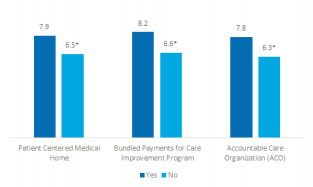
Note: *Significantly lower than hospitals that participated in the respective CMS payment program (p<0.05). The sample consists of 3,599 non-federal acute care hospitals. There are 10 measures of EHR data use to inform clinical practice.
- Hospitals that participated in quality programs of The Center for Medicare and Medicaid Innovation (CMMI) within the Centers for Medicare and Medicaid Services (CMS) used their EHR data on average in 8 ways, compared to hospitals that did not participate in these programs that used their data on average in 6 ways.
- Participants of the CMMI Bundled Payment Program had the highest rates, 8.2, of EHR data use to inform clinical practice.
- Hospitals that did not participate in the Accountable Care Organization Model had the lowest rates of EHR data use, 6.3 processes.
Summary
EHRs allow for a more seamless flow of information by leveraging digital technologies that can transform the way that care is delivered and compensated (2). EHRs aggregate patient information, such as medical and immunization history, diagnoses, medications, treatment plans, allergies, radiology images, and laboratory and test results, so providers can have a more complete picture of a patient and make well-informed care decisions quickly (2). This patient information can then be used by hospitals to inform their clinical practice patterns to improve care and reduce safety risks (2).
Since 2015, the majority of hospitals have used electronic clinical data from their EHR for internal hospital processes that inform clinical practice. In 2017, 94 percent of hospitals used their data in at least one way. The most common uses of EHR data in 2017 were supporting a continuous quality improvement process (82 percent), monitoring patient safety (81 percent of hospitals), and creating a dashboard with measures of organizational performance (77 percent). EHR data is least commonly used to develop an approach to query for patient data (51 percent), assess adherence to clinical practice guidelines (59 percent), and identify care gaps for specific patient populations (60 percent).
On average, hospitals used their EHR data in 7 different ways. However, the use of clinical data varied by hospital characteristics. Medium and large hospitals, non-critical access hospitals, hospital systems, non-profit hospitals, teaching hospitals, and those located in urban settings had the highest use of the EHR data. The largest improvements in the use of EHR data over time occurred in for-profit hospitals, which, in aggregate, engaged in 4 additional measures of EHR data use between 2015 and 2017. In general, these hospital characteristics have been associated with early adoption of health information technology and higher rates of interoperability (4). There was also substantial variation in the use of EHR data by developer. Most hospitals with Epic, Meditech, and Cerner used their EHR data to perform the majority of processes that inform clinical practice, but this did not occur among hospitals with other EHR developers.
Hospitals that engaged in the interoperability domains, meaning they could send, find, receive, or integrate summary of care records, had the highest rates of EHR data use. For example, hospitals that could send summary of care records used their EHR data on average for 7 out of 10 measures. This was significantly higher than hospitals that could not send summary of care records, which used their EHR data on average for 4 out of 10 measures. Hospitals that could send, find, receive, and integrate summary of care records had the highest rates of EHR data use. These hospitals used their electronic clinical information for approximately 9 out of the 10 measures.
Participation in CMS Innovation Models was also positively associated with greater use of EHR measures. Hospitals participating in a CMS program used their EHR data in approximately 8 ways, while hospitals that did not participate in any of these programs used their data on average in 6.5 ways. Hospitals participating in the Bundled Payments for Care Improvement Program had the highest rates of using their EHR data, 8.2 ways.
Across all hospital types, there was a significant increase in the use of EHR data from 2015 to 2016. The trend towards greater use of EHR data is likely to continue with the forthcoming implementation of the 21st Century Cures Act. For example, hospitals’ adoption of the 2015 Edition of health IT certification criteria (2015 Edition); which includes updates to technical requirements to facilitate greater interoperability and enable the exchange of health information, might lead to increased use of EHR data. Thus, understanding how hospitals are currently using their EHR data is important as policy initiatives seek to incentivize hospitals to use their EHR data for performance and population health management.
Definitions
EHR use: A hospital reports they employed at least one of ten possible measures that describe hospital processes for leveraging data within their EHR to inform clinical practice (see appendix for survey question).
Non-federal acute care hospital: Hospitals that meet the following criteria: acute care general medical and surgical, children’s general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or state/local government and located within the 50 states and District of Columbia.
Small hospital: Non-federal acute care hospitals of bed sizes of 100 or less.
Rural hospital: Hospitals located in a non-metropolitan statistical area.
Critical Access Hospital: Hospitals with less than 25 beds and at least 35 miles away from another general or critical access hospital.
Interoperability: The ability of a system to exchange electronic health information with and use electronic health information from other systems without special effort on the part of the user (3). This brief further specifies interoperability as the ability for health systems to electronically send, receive, find, and use health information with other electronic systems outside their organization.
Integrate: Whether the EHR integrates summary of care record received electronically (not eFax) from providers or sources outside your hospital system/organization without the need for manual entry.
Find: Whether providers at your hospital query electronically for patients’ health information (e.g., medications, outside encounters) from sources outside of your organization or hospital system.
Data Source and Methods
Data are from the American Hospital Association (AHA) Information Technology (IT) Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to measure the adoption and use of health IT in U.S. hospitals. ONC funded the 2015-2017 AHA IT Supplements to track hospital adoption and use of EHRs and the exchange of clinical data.
The chief executive officer of each U.S. hospital was invited to participate in the survey regardless of AHA membership status. The person most knowledgeable about the hospital’s health IT (typically the chief information officer) was requested to provide the information via a mail survey or secure online site. Non-respondents received follow-up mailings and phone calls to encourage response.
The 2015 survey was fielded from October 2015 to the end of February 2016. The response rate for non-federal acute care hospitals was 56%. The 2016 survey was fielded from October 2016 to the end of February 2017. The response rate for non-federal acute care hospitals was 58%. The 2017 survey was fielded from the beginning of January 2018 to the middle of May 2018. The response rate for non-federal acute care hospitals was 64 percent. A logistic regression model was used to predict the propensity of survey response as a function of hospital characteristics, including size, ownership, teaching status, system membership, and availability of a cardiac intensive care unit, urban status, and region. Hospital level weights were derived by the inverse of the predicted propensity.
Estimates considered unreliable had a relative standard error adjusted for finite populations greater than 0.49. Responses with missing values were assigned zero values. Significant differences were tested using p < 0.05 as the threshold.
References
1. Henry, J., Pylypchuk, Y., Searcy T. & Patel V. (May 2016) Adoption of Electronic Health Record Systems among U.S. Non-Federal Acute Care Hospitals: 2008-2015. ONC Data Brief, no.35. Office of the National Coordinator for Health Information Technology: Washington DC.
2. Office of the National Coordinator for Health Information Technology. (October 2017) Benefits of EHRs.
3. Centers for Medicare and Medicaid Services. Innovation Models. .
4. Pylypchuk Y., Johnson C., Henry J. & Ciricean D. (November 2018). Variation in Interoperability among U.S. Non federal Acute Care Hospitals in 2017. ONC Data Brief, no.42. Office of the National Coordinator for Health Information Technology: Washington DC.
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division and Talisha Searcy, Branch Chief of the Data Analysis Branch.
Suggested Citation
Parasrampuria S. & Henry J. (April 2019) Hospitals’ Use of Electronic Health Records Data, 2015-2017, no.46. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix
Appendix Table A1: Survey questions assessing use of EHR data to inform clinical practice and variation in interoperability among hospitals.
| Question Text | Response Options |
|---|---|
| Please indicate whether you have used electronic clinical data from the EHR or other electronic system in your hospital to:(Please check all that apply) |
|
| When a patient transitions to another care setting or organization outside your hospital system, how often does your hospital use the following methods to send a summary of care record? |
Often | Sometimes| Rarely | Never | Don’t Know/NA Methods without intermediaries
|
| When a patient transitions to another care setting or organization outside your hospital system, how often does your hospital use the following methods to receive a summary of care record? |
Often | Sometimes| Rarely | Never | Don’t Know/NA Methods without intermediaries
|
| Do providers at your hospital query electronically for patients’ health information (e.g. medications, outside encounters) from sources outside of your organization or hospital system? |
|
| Does your EHR integrate the information contained in summary of care records received electronically (not eFax) without the need for manual entry? This could be done using software to convert scanned documents into indexed, discrete data that can be integrated into EHR. |
|
