In this section
Learn how to:
- Understand Value-Based Care
- Prepare your practice for the Quality Payment Program (QPP)
- Understand the Merit-Based Incentive Payment System (MIPS)
- Understand Alternative Payment Models (APMs)
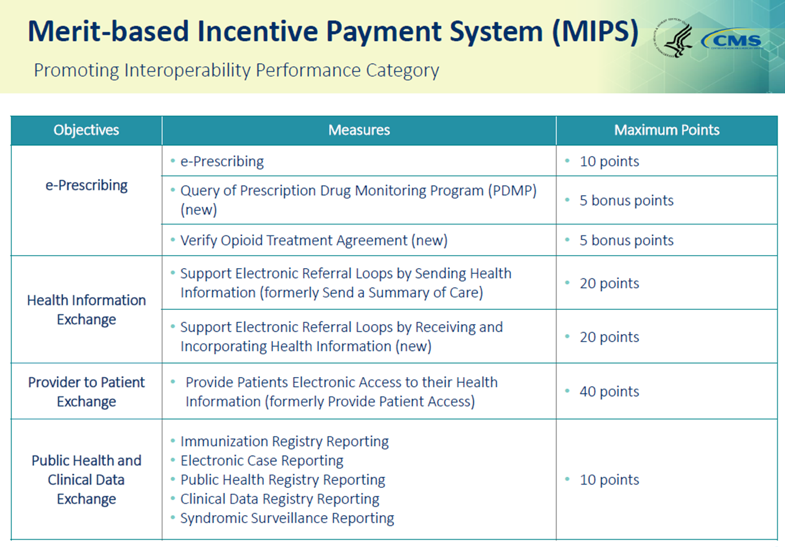
- Understand the Promoting Interoperability performance category
- Find support for small practices
- Strengthen primary care with the CMS Primary Cares Initiative and Comprehensive Primary Care Plus (CPC+)
Traditional fee-for-service pays primarily for specific, itemized care delivered by clinicians. This approach has a number of potentially adverse effects, such as:
- rewarding the volume rather than the quality of care;
- putting emphasis on treatment at the expense of prevention and wellness;
- providing no incentives for integrating and coordinating care; and
- discouraging practice transformation and clinician-driven innovation.
Changes in healthcare payment, arising in part from the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), have focused on redesigning healthcare payment so that it rewards better quality care, increases cost effectiveness, ensures appropriate compensation for patient-centered care, and supports both practice improvements and clinician-driven innovations in care delivery.
This alternative to traditional fee-for-service is Value-Based Care, supported by CMS Value-Based programs.