An official website of the United States government
Here’s how you know
Official websites use .gov
A
.gov
website belongs to an official government organization in the
United States.
Secure .gov websites use HTTPS
A
lock
(
) or
https://
means you’ve safely connected to the .gov website. Share sensitive
information only on official, secure websites.
TEFCA Awareness and Planned Participation Among U.S. Hospitals: 2023
No. 72 | July 2024
A critical provision of the 21st Century Cures Act, the Trusted Exchange Framework and Common AgreementTM (TEFCATM) was published in 2022. The purpose is to facilitate nationwide connectivity by enabling the exchange of electronic health information across networks.1 The three goals of TEFCA are to (1) to establish a universal governance, policy, and technical floor for nationwide interoperability; (2) to simplify connectivity for organizations to securely exchange information to improve patient care, enhance the welfare of populations, and generate health care value; and (3) to enable individuals to gather their health care information.2 The first set of Qualified Health Information NetworksTM (QHINsTM) were approved to implement TEFCA and began exchanging data in late 2023. Participation in TEFCA is not mandated by law, so it is important to assess the extent to which health care providers, as critical TEFCA participants, are aware of and plan to participate in TEFCA. This data brief uses nationally representative survey data from the 2022 and 2023 American Hospital Association (AHA) Information Technology (IT) supplement to explore non-federal acute care hospitals’ awareness and plans to participate in TEFCA.
Highlights
- Over 60 percent of hospitals were aware of TEFCA and planned to participate in 2023, an increase from 51 percent in 2022.
- Approximately 7 out of 10 hospitals that participated in national networks or health information exchanges (HIEs) planned to participate in TEFCA, compared to 4 out of 10 hospitals that did not participate in either type of network.
- Hospitals with more resources, such as those that are larger, non-critical access, and affiliated with health systems, indicated greater awareness and had higher levels of planned participation in TEFCA when compared to smaller, critical access, and independent hospitals with fewer resources.
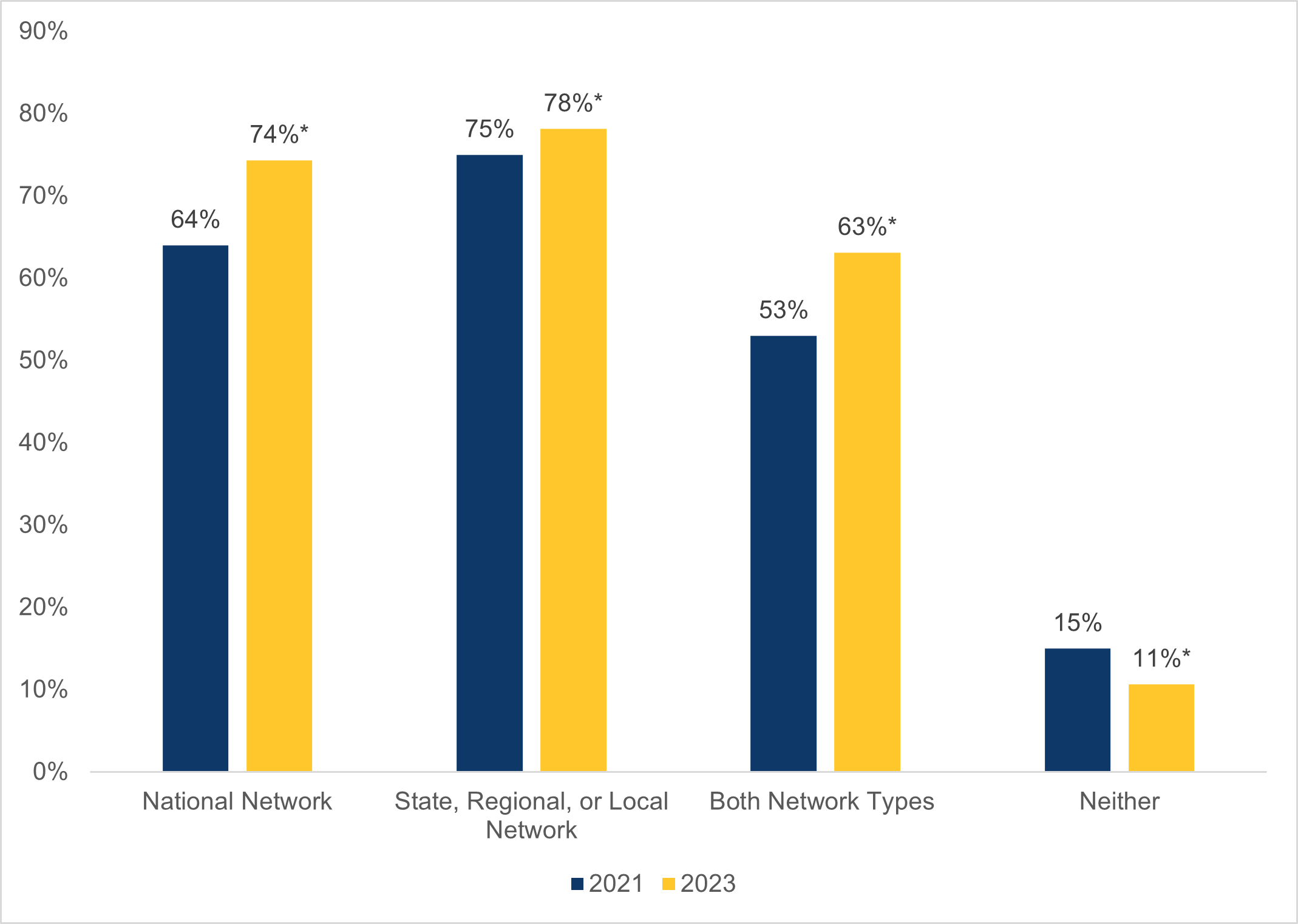
In 2023, over 60 percent of hospitals were aware of and planned to participate in TEFCA, an increase from 51 percent in 2022.
Findings
- Among hospitals that were aware of TEFCA, 85% planned to participate as of 2023, an increase from 69% in 2022.
- The percent of hospitals that were aware of TEFCA but did not know if they would participate decreased from 23% to 9% from 2022 to 2023.
- Around 1 out of 4 hospitals were not aware of TEFCA, with no change in awareness from 2022.
Figure 1: Percent of non-federal acute care hospitals and their awareness and plans to participate in TEFCA, 2022-2023.
Notes: Denominator represents all non-federal acute care hospitals that provide inpatient care. Missing responses were excluded from the denominator (n=114 for 2022; n=121 for 2023). See the Definitions section for further clarification regarding TEFCA participation. Also see survey questions used to inform these definitions in Appendix Table A1. *Significantly different from 2022 within a corresponding category (p<0.05).
Between 2022 and 2023, hospitals with greater resources reported greater increase in their awareness and plans to participate in TEFCA compared to their less well-resourced counterparts.
Findings
- Among hospitals that were aware of TEFCA, there were increases in plans to participate in TEFCA across all types of hospitals.
- Hospitals with greater resources (e.g., multi-hospital system member, medium to large) increased their awareness and plans to participate in TEFCA at higher rates compared to their less well-resourced counterparts.
- Although critical access hospitals and rural hospitals’ plans to participate in TEFCA increased between 2022 and 2023, their levels of awareness and plans to participate were still lower when compared to their suburban, urban, and non-critical access counterparts.
Table 1: Percentage point change in awareness and plans to participate in TEFCA by hospital characteristics, 2022-2023.
| Aware of TEFCA and plan to participate | Aware of TEFCA but not planning to participate | Aware of TEFCA and do not know if they plan to participate | Not aware of TEFCA | |||||
|---|---|---|---|---|---|---|---|---|
| 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | |
| System Affiliation | ||||||||
| Multi-Hospital System Member (67%) | 77 | +16 | 3 | +3 | 6 | -15 | 14 | -3 |
| Independent Hospital (33%) | 37 | +8 | 3 | +1 | 15 | -11 | 46 | +3 |
| Critical Access | ||||||||
| Critical Access Hospital (31%) | 42 | +10 | 5 | +4 | 11 | -16 | 41 | +2 |
| Non-Critical Access Hospital (69%) | 73 | +14 | 2 | +1 | 8 | -13 | 16 | -3 |
| Bedsize | ||||||||
| Small (52%) | 52 | +12 | 4 | +2 | 10 | -15 | 34 | 0 |
| Medium or Large (48%) | 77 | +15 | 3 | +2 | 8 | -13 | 13 | -3 |
| Urban/rural | ||||||||
| Rural (27%) | 46 | +9 | 4 | +3 | 12 | -11 | 38 | 0 |
| Suburban-Urban (57%) | 73 | +16 | 3 | +2 | 7 | -17 | 17 | -1 |
Notes: Missing responses were excluded from the denominator (n=114 for 2022; n=121 for 2023). Please refer to the Definitions section of this data brief for more information on the terminology.
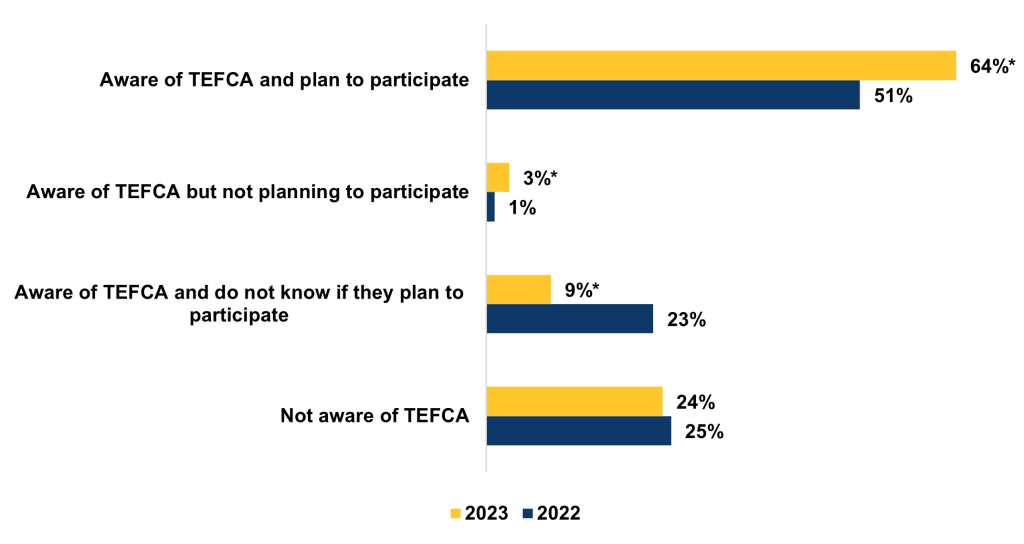
75% of hospitals that participated in at least one national network and 69% of hospitals that participated in at least one regional network planned to participate in TEFCA compared to 39% of hospitals that did not participate in either.
Findings
- There was a 29 percentage point increase from 2022 to 2023 in hospitals’ plans to participate in TEFCA and a 13 percentage point increase in awareness of TEFCA among hospitals that are not participating in either national networks or state, regional, or local networks.
- Seventy-nine percent of routinely interoperable hospitals planned to participate in TEFCA compared to just 28% of hospitals that are not fully interoperable.
- There was a 26 percentage point increase from 2022 to 2023 among sometimes interoperable hospitals in their plans to participate in TEFCA.
- Lack of awareness of TEFCA was highest among hospitals that didn’t participate in any type of network or that were not fully interoperable.
Table 2: Percentage point change in awareness and plans to participate in TEFCA by network participation and interoperability engagement, 2022-2023.
| Aware of TEFCA and plan to participate | Aware of TEFCA but not planning to participate | Aware of TEFCA and do not know if they plan to participate | Not aware of TEFCA | |||||
|---|---|---|---|---|---|---|---|---|
| 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | 2023(%) | Change from 2022 (ppt) | |
| Network Participation | ||||||||
| National Network (65%) | 75 | +11 | 2 | +1 | 8 | -12 | 15 | +1 |
| State, Regional, or Local Network (78%) | 69 | +15 | 3 | +2 | 9 | -15 | 19 | -2 |
| Both Network Types (57%) | 79 | +13 | 1 | +1 | 7 | -14 | 13 | -1 |
| Neither (14%) | 39 | +29 | 3 | -2 | 5 | -15 | 53 | -13 |
| Interoperability Engagement | ||||||||
| Routinely Interoperable (43%) | 79 | +7 | 4 | +4 | 7 | -10 | 10 | -1 |
| Sometimes Interoperable (27%) | 76 | +26 | 2 | +1 | 7 | -23 | 15 | -4 |
| Not Fully Interoperable (30%) | 28 | +6 | 3 | +1 | 14 | -9 | 55 | +2 |
Notes: Missing responses were excluded from the denominator (n=114 for 2022; n=121 for 2023). Hospitals were categorized as participating in a national network if they indicated participating in at least one of three national networks: Carequality, CommonWell Health Alliance, and eHealth Exchange. Please refer to the Definitions section of this data brief for additional definitions.
Interoperability status and network participation were major predictors of awareness and plans to participate in TEFCA.
Findings
- The most influential predictor of TEFCA awareness and participation was interoperability engagement. Those hospitals that routinely or sometimes were interoperable had higher rates of TEFCA awareness when compared to those hospitals that were not fully interoperable.
- For those hospitals that were routinely or sometimes interoperable, network participation and ownership status were major predictors of awareness and plans to participate in TEFCA.
- For those hospitals that were not fully interoperable, critical access hospital status and network participation were major predictors of awareness and plans to participate in TEFCA.
Figure 2: Major predictors of awareness and plan to participate in TEFCA.
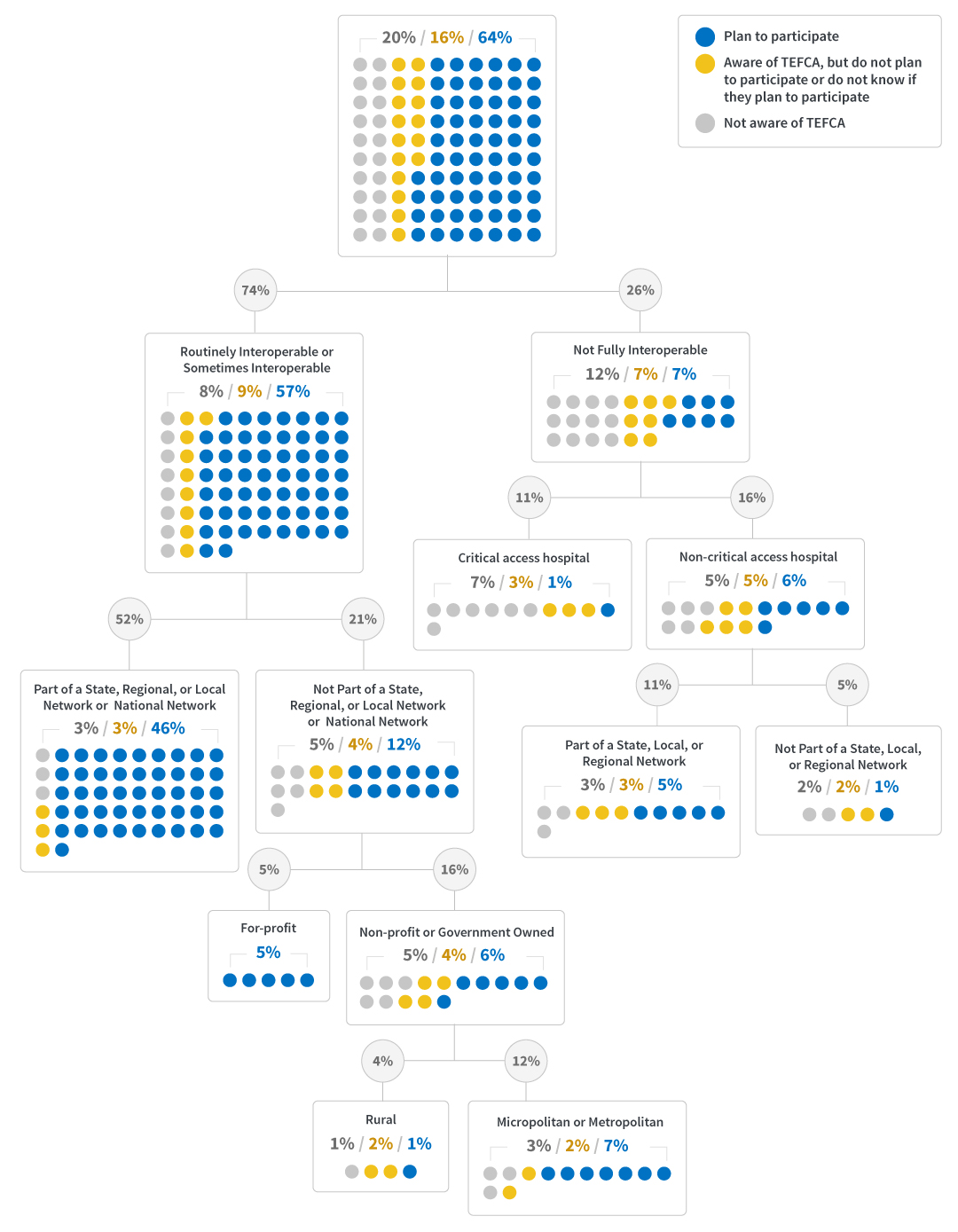
Notes: Nodes may not add up to the one above due to rounding. Decision tree created automatically using tidymodels in R and a recursive partitioning (rpart) classification model to select the most influential hospital characteristics.
Summary
TEFCA aims to enhance the nationwide exchange of health information by enabling the exchange of electronic health information across networks.(1) Broad participation by health care organizations will be essential to achieve widespread exchange. In 2023, more than 60% of hospitals planned to participate in TEFCA, an increase from 51% in 2022. Planned participation also increased, with only 9% of hospitals aware of TEFCA indicating that they did not have plans to participate, down from 23% in 2022. The growth in planned TEFCA participation between 2022 and 2023 among non-federal acute care hospitals aligns with the start of exchange activities and the designation of the first Qualified Health Information Networks (QHINs),3 suggesting a growing recognition among hospitals of the potential benefits that TEFCA offers.
However, while most hospitals that were aware of TEFCA planned to participate in it, one quarter of hospitals reported that they were not aware of TEFCA, unchanged from 2022. This highlights the essential need for further education and outreach about TEFCA to ensure that hospitals and smaller health care organizations are knowledgeable about its benefits and costs and how they might participate in it, even within networks in which they are already participants.
Correlations between hospital characteristics and their knowledge of and plans to participate in TEFCA highlight a division between organizations planning to participate and those unaware of TEFCA. Among hospitals aware of TEFCA, hospitals’ plans to participate in TEFCA increased across all hospital types; however, the level of growth varied by hospital characteristics. Hospitals with more resources, such as those affiliated with health systems and with larger bed sizes, indicated greater awareness and had higher planned participation levels in TEFCA when compared to smaller, critical access, and independent hospitals with fewer resources.
Hospitals participating in national or regional networks were much more likely to report planning to participate in TEFCA compared to the 14% of hospitals not involved in any network type. By participating in TEFCA, hospitals can join a QHIN or become subparticipants under a participant, both of which include existing national networks and some regional HIEs. Our findings underscore the importance of prior network involvement in shaping hospitals’ participation in TEFCA, possibly due to existing technical capabilities, the need for data exchange, and familiarity with electronic health information exchange.
While the gap in plans to participate between hospitals already in networks and those not in any network remained large in 2023, we did observe a substantial increase in the proportion of hospitals without prior network involvement planning to participate in TEFCA. In 2022, only 10% of these hospitals planned to participate in TEFCA, which increased by 29 percentage points to 39% in 2023. This trend is important because it indicates net-new participation in network-based exchange through participation in TEFCA. It will be important to monitor this trend over time. It will be particularly critical to evaluate trends in participation because the statistic for non-network participants is an outlier.
In April 2024, ONC published Version 2.0 of the Common Agreement,2 which incorporated the Health Level Seven (HL7®) Fast Healthcare Interoperability Resources (FHIR ®) standard to enhance interoperability and API scalability.4 With the continued release of key policies and designation of additional QHINs guiding hospitals’ participation in TEFCA, it will be important to keep tracking hospitals’ awareness and plans to participate in TEFCA. These efforts are essential in ensuring that hospitals, regardless of resources such as size, system affiliation, or prior network participation, can participate and benefit from the nationwide connectivity that TEFCA aims to achieve. Enhancing nationwide health information exchange is complex and requires collaboration from all stakeholders across the health care continuum.
Definitions
Critical Access Hospital: Hospitals with less than 25 beds and at least 35 miles away from another general or critical access hospital.
Sometimes Interoperable: Non-federal acute care hospitals were not routinely interoperable, and therefore reported finding, sending, receiving electronic patient health information often or sometimes, and integrating (but not routinely) electronic patient health information from sources outside their hospital or hospital system.
Interoperability: The ability of a system to exchange electronic health information with and use electronic health information from other systems without special effort on the part of the user. This brief further specifies interoperability as the ability for health systems to electronically send, receive, find, and integrate health information from electronic systems outside their organization.
National Network: Health information networks that are nationwide in scope. Hospitals were categorized as participating in a national network if they indicated participating in at least one of three national networks: Carequality, CommonWell Health Alliance, and eHealth Exchange. This includes multi-EHR vendor networks, which can be used to exchange health information either directly through an EHR or health information exchange (HIE) vendor.
Non-federal Acute Care Hospital: Hospitals that meet the following criteria: acute care general medical and surgical, children’s general, and cancer hospitals owned by private/not-for-profit, investor-owned/for-profit, or state/local government and located within the 50 states and District of Columbia.
Not Fully Interoperable: Non-federal acute care hospitals that reported rarely or never finding, sending, and receiving electronic health information and did not integrate electronic patient health information from sources outside their hospital or hospital system.
Routinely Interoperable: Non-federal acute care hospitals that were routinely or often interoperable, and reported they often find, often send, often receive, and routinely integrate electronic patient health information from sources outside their hospital or hospital system.
Rural Hospital: Hospitals located in a non-metropolitan core-based statistical area
Large Hospital: Non-federal acute care hospitals with bed sizes of 400 or more.
Medium Hospital: Non-federal acute care hospitals with bed sizes of 100-399.
Small Hospital: Non-federal acute care hospitals with bed sizes of 100 or less
System-affiliated Hospital: A system is defined as either a multi-hospital or a diversified single hospital system. A multi-hospital system is two or more hospitals owned, leased, sponsored, or contract managed by a central organization. Single, freestanding hospitals may be categorized as a system by bringing into membership three or more, and at least 25 percent, of their owned or leased non-hospital pre-acute or post-acute health care organizations.
TEFCA Participant: Participants may include persons or entities that have entered into a contract to participate in a QHIN. Some examples of Participants could include, but are not limited to, a HIN, a health system, a health IT developer, a payer, or a federal agency.5
TEFCA Subparticipant: Subparticipants may include persons or entities that use the services of a Participant to send and receive EHI. For example, if a QHIN is composed of health information exchanges, the health information exchange would be the Participant, and those who use the health information exchange services, (such as health systems, ambulatory providers, health IT developers, payers, and others) are the subparticipants.5
Data Sources and Methods
Data are from the 2022 and 2023 American Hospital Association (AHA) Information Technology Supplement to the AHA Annual Survey. Since 2008, ONC has partnered with the AHA to measure adoption and use of health IT in U.S. hospitals. ONC funded the 2022 and 2023 AHA IT Supplement to track hospital reported network and TEFCA participation.
The chief executive officer of each U.S. hospital was invited to participate in the survey regardless of AHA membership status. The person most knowledgeable about the hospital’s health IT (typically the chief information officer) was requested to provide the information via a mail survey or secure online site. Nonrespondents received follow-up mailings and phone calls to encourage response.
This brief reports results from the 2021-2023 AHA IT Supplement. Due to pandemic-related delays, the 2020 survey was not fielded on time and was fielded from April 2021 to September 2021; the 2022 survey was fielded from July 2022 to December 2022; and the 2023 survey was fielded from March 2023 to August 2023. Since the IT supplement survey instructed respondents to answer questions as of the day the survey is completed, we refer to responses to the 2020 IT supplement survey as happening in 2021 in this brief. Of note, the 2022 and 2023 surveys were fielded relatively close together (July to December 2022 and March to August 2023) to catch up from pandemic-related delays. For the 2023 survey, the response rate for non-federal acute care hospitals (N = 2,547) was 58%.
A logistic regression model was used to predict the propensity of survey response as a function of hospital characteristics, including size, critical access hospital status, location, system affiliation, teaching status, ownership, and EHR certification status. Hospital-level weights were derived by the inverse of the predicted propensity.
For more information on methods related to send, find, receive, and integrate domains, please refer to the data sources and methods section detailed in a previous data brief.6
References
- The Sequoia Project. What Is the ONC Trusted Exchange Framework and Common Agreement? 2023 [Available from: https://rce.sequoiaproject.org/tefca/.
- The Office of the National Coordinator for Health Information Technology (ONC). Trusted Exchange Framework and Common Agreement (TEFCA) 2024 [Available from: https://healthit.gov/policy/tefca/.
- United States Department of Health and Human Services. HHS Marks Major Milestone for Nationwide Health Data Exchange 2023 [Available from: https://www.hhs.gov/about/news/2023/12/12/hhs-marks-major-milestone-nationwide-health-data-exchange.html.
- Knee M, Henry J. The Office of the National Coordinator for Health Information Technology (ONC). 2023. Available from: https://healthit.gov/blog/insights-updates/coming-in-hot-tefca-will-soon-be-live-and-add-support-for-fhir-based-exchange/.
- The Sequoia Project. How Can I Participate in TEFCA? 2023 [Available from: https://rce.sequoiaproject.org/participate/#WhatisanIndividualUser.
- Gabriel MH, Richwine C, Strawley C, Barker W, Everson J. Interoperable Exchange of Patient Health Information Among U.S. Hospitals, 2023. Office of the National Coordinator for Health Information Technology: Washington DC. Data Brief: 71. 2024.
Acknowledgments
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division, Vaishali Patel, Deputy Director of the Technical Strategy and Analysis Division, and Wesley Barker, Chief of the Data Analysis Branch with subject matter expertise from Kimberly Tavernia and Lori Haberman.
Suggested Citation
Chang, W., Gabriel, MH., Everson, J. (July 2024). Network and TEFCA Participation among Non-Federal Acute Care Hospitals, 2023. ONC Data Brief, no.72. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix
Appendix Table A1: Network and TEFCA survey questions in the 2023 American Hospital Association (AHA) Information Technology Supplement Survey
| Question Text | Response Options |
|---|---|
| 9. Which of the following national health information exchange networks does your hospital currently actively participate in (i.e., operational exchange)? Check all that apply |
|
| 10. Are you aware of the Trusted Exchange Framework and Common Agreement (TEFCA)? |
|
| 11. If yes, are you currently participating or do you plan to participate in TEFCA exchange (such as through your HIE or other national network)? |
|
Appendix Figure A2: Percent of non-federal acute care hospitals that participate in national and state, regional, or local health information networks, 2021 vs 2023.