Over the last several weeks we have been following Larry (Part 1, Part 2, Part 3), a patient with diabetes and a history of non-compliance. Because Larry’s primary care providers either do not have EHRs or other care coordination tools or are unable to exchange information between one another, they do not know that he had been hospitalized and instructed to make important changes in his medications.
Larry’s primary care providers also didn’t know that Larry was colonized with methicillin‐resistant Staphylococcus aureus (MRSA)—and neither did the hospital where he was admitted. In the weeks following his in-patient stays, the hospital experienced an increase in MRSA infection rates.
Larry’s story is just one of a number of stories reported in recent years about patients infected by MRSA. These have grabbed headlines because of the threat this germ poses to hospital patients and public health, and the increased focus on MRSA prevention in the hospital setting.
Hospital-acquired MRSA can be frightening, as it:
- Causes severe and sometimes life-threatening infections (often located in the blood stream, organs, or at the site of a recent surgery).
- Is generally transmitted from patient to patient through surface contamination and the contaminated hands of health care workers.
Also, MRSA prevention is difficult because patients colonized (carrying, but not infected) with MRSA often do not show physical symptoms, making it difficult for many hospitals to proactively identify these patients and take precautionary measures before infections occur.
Hospitals nationwide are working to develop systems focused on MRSA prevention, with varying degrees of success.
A Breakthrough MRSA Prevention Approach in Indianapolis Hospitals
Several hospitals in Indianapolis, however, have implemented an approach that is showing big results—from which they hope other hospitals and health care providers can benefit. By using electronic care coordination tools that allow hospital staff to be smarter and more efficient in their MRSA prevention efforts, they’ve sustained a reduction in MRSA infection rates of more than 30%.
MRSA Prevention: A 2 Pronged Approach
The hospitals in Indianapolis implemented a 2 pronged approach, which focused on alerting key points of contact about individuals with MRSA, and creating organization-wide change plans to encourage adoption of the new MRSA prevention system.
1: Identify MRSA-colonized patients as soon as they are admitted
Working together, Indiana University, the Regenstrief Institute, and several Indianapolis hospitals knew they needed to arm health care providers with information that would help them identify MRSA-colonized patients like Larry as soon as they checked into area hospitals.
“We needed to step up and take ownership of the problem of avoidable infections. Managing information between hospitals and other health care venues is just one method. Hospitals deciding that it’s in their best interest to cooperate and share promising practices with one another would be a boon in other cities, too. Zero tolerance of avoidable infections!” said Dr. Bill Tierney, President & CEO, Regenstrief Institute.
Using a clinical informatics network was essential
The team, led by Dr. Brad Doebbling, knew the Indiana Network for Patient Care (INPC)—an existing local clinical informatics network operated by the Indiana Health Information Exchange (IHIE)—contained a wealth of information from its care coordination tools that could help hospital staff identify MRSA-colonized or -infected patients at the point of care.
In addition to serving as an enormous repository of data, the INPC also includes electronic notification functionality, which allows hospitals to send Admission, Discharge and Transfer (ADT) messages to the INPC when patients are admitted to participating hospitals or emergency departments and query for (and return) information that may be relevant to the treatment of the patient.
The team created a MRSA registry
Because the INPC had not been used systematically for MRSA prevention in the past, the team had to create a MRSA registry to pinpoint patients with a history of MRSA colonization or infection. Dr. Abel Kho, MD, a Regenstrief Affiliated Scientist at Northwestern University, joined and led the team through the process of developing this registry with data from multiple sources, such as infection preventionists and hospital, regional and commercial labs.
Automated Alerts were established to identify MRSA-colonized patients
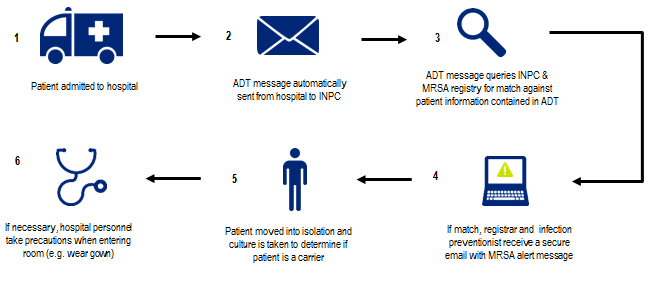
Once the MRSA registry was created, the team configured INPC’s existing electronic notification system to automatically alert key points of contact at participating Indianapolis hospitals about MRSA risks. The workflow is outlined in Figure 1.
FIGURE 1: MRSA Electronic Notification System Workflow
2: Promoting organizational system change to increase MSRA prevention
Indiana’s data sharing strategy was coupled with an organizational system change initiative to help identify, adopt, and improve adherence to effective MRSA prevention techniques such as hand washing and putting patients in isolation.
- The Plexus Institute supplied organizational change coaches to participating hospitals and trained hospital staff on how to use lean and positive deviance approaches to engage other staff in behavior change and effectively use the alerts for MRSA prevention.
- Participating hospitals contributed to an internal blog and participated in weekly calls to share promising practices and lessons learned.
- MRSA prevention teams in each hospital implemented new, innovative techniques.
- For example, one hospital began tracking the supplies used to isolate a patient by unit in order to evaluate whether certain units were using isolation approaches more frequently than others.
- Similarly, another hospital worked closely with the housekeeping staff to identify opportunities for improving the decontamination of rooms.
The result? MRSA infection rates fell
The results of these efforts are remarkable. As participating hospitals witnessed an increase in recommended practices, their MRSA infection rates fell.
- Between 2009 and 2010, participating hospitals experienced an 85% reduction in the rate of MRSA infections compared to their baseline period, and reductions have remained 32% lower than baseline.
- Since inception, the program has delivered 16,000 MRSA notifications on over 10,000 patients across 17 different hospitals in Indiana.
- 25% of these alerts were sent to hospitals where the patient had no recorded history of MRSA; without the alert, the patient’s history of MRSA colonization/infection would have been very difficult, if not impossible, to identify.
If Larry had been admitted to one of these Indiana hospitals, there is a high likelihood they would have known of his MRSA colonization and taken the appropriate MRSA prevention precautions to prevent infections from occurring.
To learn more about Indiana’s efforts to reduce MRSA infection rates and improve care coordination, check out the full implementation brief on the Bright Spots website.
How have you seen your state use health information exchange in care coordination or deploy unique tactics to prevent the spread of MRSA? Please share your comments below.




