Introduction
About this playbook
The Patient Engagement Playbook is a tool for clinicians, health care practice staff, hospital administrators, and others who want to leverage health IT — particularly electronic health record (EHR) patient portals — to engage patients in their health and care.
Why the focus on patient engagement? Because engaged patients have the knowledge, skills, ability, and willingness to manage their health and care and to act on clinicians’ recommendations. Practices that invest in health IT for patient engagement can expect returns in the form of better outcomes and lower costs.
When selecting an EHR vendor, keep patients in mind.
Before you contract with an EHR vendor, be sure to research the EHR market (including competing vendors, products, and services) and make a priority list of features you want in your EHR.
Health care practices across the country are already seeing the benefits of EHR patient portal implementation on patient engagement and beyond. The rewards are real: more informed, involved patients; more effective delivery of care; and reduced burden on office staff. But the barriers are real, too: cumbersome enrollment; clunky interfaces; reluctant patients and office staff; and questions of privacy and security. It will take years to address all of the pain points, but transformation is underway.
How to use the Playbook
In this playbook, we demystify patient portals and describe how you can make them work for you and your patients.
If your practice is just getting started with a patient portal, use the Playbook to learn how to promote it and establish processes that drive adoption — including how to:
- Make enrollment easier on your practice (1.1, 1.2)
- Promote the portal and register patients in the office (Chapter 1 graphic, 1.3)
- Educate patients about the portal and include it in visit summaries (1.4)
If your practice has already established a patient portal, use the Playbook to get ideas and tips for establishing features and policies that streamline and improve care — such as:
- Communicate with patients by email and share notes through the portal (2.2, 2.3)
- Navigate proxy access with patients and their caregivers (4.1)
- Create a plan for integrating patient-generated health data into your practice (5.1)
- Build goodwill for the portal among clinicians and staff (1.4)
- Activate features like online booking (2.1)
- Set up an efficient workflow for collecting family health histories (5.2)
We’ve compiled best practices and home-grown solutions from innovative clinicians, practice administrators, and health systems around the country.
We’ve also told their stories in “From the field” examples scattered throughout the Playbook. The highlighted organizations stand out as pioneers — they’ve piloted unique programs that leverage health IT, shown how using health IT strategically can produce results, and earned national attention from the press and fellow industry leaders.
Each “From the field” example sheds light on what it means to put the Playbook into practice. There’s much to learn from analyzing these bright spots and scaling their success. Even a few small changes in your practice and patient portal implementation can lead to meaningful improvements in portal adoption, care delivery, and health outcomes.
Every day, clinicians and practices embrace new technologies, discover ways to improve care, and find opportunities for meaningful patient connection. As health IT and health care delivery evolve, the Playbook will evolve too. Over time, we’ll update it to include a broader range of tried-and-true strategies for involving patients in their health and care.
Why a playbook?
Playbooks aren’t static instruction manuals — they’re always-evolving sets of strategies and approaches. Good coaches update their playbooks constantly, and each iteration reflects new, innovative solutions to shifting circumstances.
This playbook is an important tool for our mission to help clinicians and their patients adopt and adapt to patient portals and patient-generated health data. We hope you’ll use it in a way that works for you and your practice.
For example, you may want to:
- Review patient portal benefits with office staff, so they can share them with patients
- Focus on one chapter at a time — discuss lessons during team meetings, apply best practices in the workplace, and have ongoing conversations about what works and what can be improved
- Use Playbook language on your website or Facebook page to let patients know how they can use the patient portal to participate in their care
About patient portals
Patients like portals.
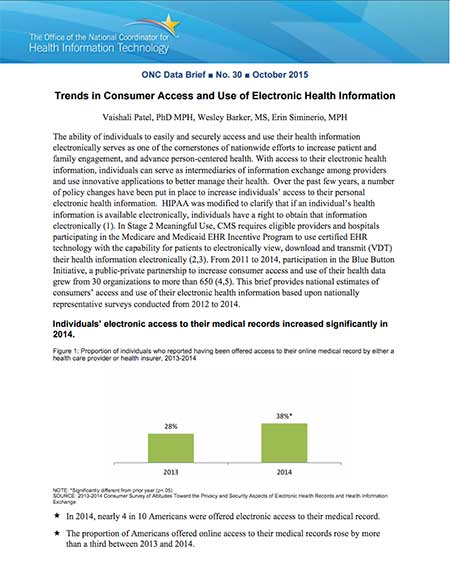
In 2017, half of Americans were offered access to an online medical record. 8 in 10 individuals who accessed their record reported it was both easy to understand and useful. 3
The Centers for Medicare & Medicaid Services (CMS) launched Meaningful Use objectives to encourage clinicians and practices to use EHR technology effectively — to improve patient care and outcomes. 4 , 5 For office-based Medicare clinicians, Meaningful Use will soon be replaced by Advancing Care Information under the proposed Quality Payment Program.
Clinicians and practices must meet Meaningful Use objectives to qualify for CMS’s EHR Incentive Programs and the upcoming Quality Payment Program. For example, Meaningful Use sets goals for clinicians and practices to:
- Enable patients to view online, download, and transmit their health information within 4 business days of the information being available
- Exchange secure messages with more than 5% of patients
- Provide clinical summaries to patients or caregivers within 1 business day for more than half of office visits
In addition to financial incentives, portals can add up to big benefits in patient care. For patients with chronic diseases, engagement in patient portals has been associated with improvements in disease management. 6 Portals can also improve preventive care. Patients with portal access to screening recommendations — like when to get their next mammogram or colonoscopy — are more likely to follow through on these recommendations. 7
Ultimately, patient portals can contribute to:
- Reduced call volume
- Improved responsiveness to patients’ needs
- Lower utilization of health services
- More effective care
- Cost savings 8
Patient portals hold enormous potential to improve patient care and practice workflow. We’ve created this playbook to help you realize it — and build an effective digital strategy for patient engagement.
Terms to know
Use this glossary, adapted from the Center for Healthcare Quality and Payment, to help establish a common language with all stakeholders.
Electronic health record (EHR). An EHR — also known as an electronic medical record or EMR — is an electronic system that clinicians use to document patients’ medical and health information. A patient’s EHR may include demographic data, progress notes, medications, vital signs, medical history, immunizations, lab results, and radiology reports. Patients don’t access their own EHR.
Patient portal. A patient portal is a secure website where patients can access their medical history and other health information stored in the EHR. Using the portal, patients can typically complete forms online, communicate with clinicians, request prescription refills, pay bills, review lab results, and schedule appointments.
Help us improve this Playbook
Best practices start with clinicians and administrators like you. We want to learn more about your experiences and hear your suggestions. Tell us what’s working and what isn’t. Have you successfully boosted portal adoption in your practice? Do you have a promising product solution?
As you discover new ways to navigate patient portals, EHRs, and other health IT solutions, let us know. We update the Playbook regularly with new patient engagement strategies and real-world examples. A good playbook is never complete: it evolves and keeps getting better — but it’s only as good as the people who use it. Please send us your suggestions, questions, and strategies so we can add to this tool and improve the patient experience.
Disclaimer
References or links in this website to any specific non-federal entity, commercial product, process, service, or company do not constitute their endorsement or recommendation by the U.S. Government or HHS. HHS is not responsible for the contents of any “off-site” website linked to in this website, nor is HHS responsible for such other website’s compliance with Section 508 (accessibility).
Content last updated on: May 31, 2019
Chapter 1
Facilitate easy enrollment
In this chapter
Learn how to:
- Make the process easier for everyone by providing a simple, secure signup process
- Save patients a step and facilitate sign-ups with automatic portal enrollment
- Build in-office portal registration into your care delivery workflow
- Get staff buy-in and communicate benefits of the portal to patients
Enrollment is the first step to engagement. In signing up for the portal, becoming familiar with it, and committing to using it, patients take an active step in managing their health and care. But patients can be slow or reluctant to enroll in their EHR patient portals — and many never enroll at all.
Patients report not enrolling because they:
- Don’t remember discussing it with their clinicians
- Lack information or motivation — for example, they don’t have signup instructions or they feel too busy
- Question the value of digital communication — for example, they think it won’t be useful or they prefer phone over email
- Need computer help — for example, they don’t have computer access or skills 9
This reluctance may seem overwhelming or out of your control, but there’s a lot that clinicians and practices can do to overcome these barriers and boost registration.
In this chapter, we’ll identify best practices for getting patients enrolled in — and on board with — patient portals. You can then tailor this approach to fit your practice. For instance, clinicians in small practices who have lifelong relationships with their patients can use the portal as a tool to deepen their communication. Large health systems might train patient greeters to become portal enrollment staff. One thing is certain: whether you’re a practice of 1 or 1,000, you can achieve high portal adoption. 10
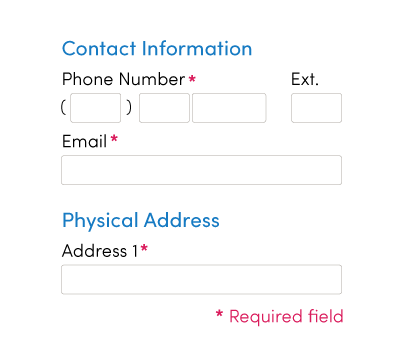
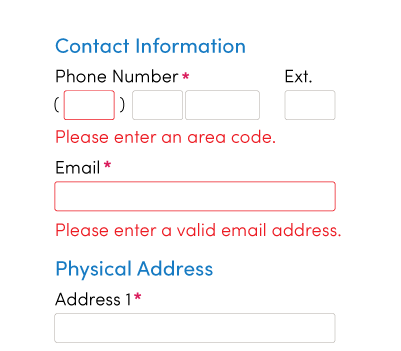
1.1 Provide simple, secure portal signup
The amount of time and effort it takes to register for a patient portal can affect whether your patients successfully enroll or give up halfway through.
Make the process easier on them and you by choosing a portal with a quick, secure signup process. Ideally, the patient has to enter only a few pieces of information — and the portal confirms the patient’s identity on the back end.
Mana Health, a health IT developer, enables patients to sign up in a few simple steps. When a patient registers, Mana’s system uses data (like demographics and the patient’s medical record number) to match up the patient with her EHR. This automated verification system means an efficient, successful enrollment process for practices and patients.
1.2 Develop an automatic enrollment policy
Facilitate enrollment!
Automatically enroll your patients in a portal account, instead of waiting for patients to sign up themselves.
To facilitate enrollment, automatically enroll your patients in a portal account, instead of waiting for patients to sign up themselves. Keep enrollment numbers up by encouraging new patients to stay registered and offering tips for patients with limited computer access or skills.
You can also increase the number of patients who enroll and use the portal by integrating portal use into patients’ care plans. For example, encourage patients to use the portal to make follow-up appointments, stay on top of recommended screenings, or request refills. Some portals even enable clinicians to create task lists for patients that include activities related to taking medications, eating a healthy diet, and staying physically active. By taking this approach, you can set the expectation that using the patient portal is part of following their recommendations — just like getting regular physical activity or taking medicine as prescribed.
athenahealth 13 | From the field
athenahealth, an EHR vendor, recommends an automatic enrollment policy. Many of athenahealth’s top 100 practices have benefited from this strategy.
“…The front office staff and physicians communicate that part of what it means to be a patient in a particular practice is using the portal. A slight shift of attitude can go a long way.
It is the difference between asking whether a patient would like to register for the portal versus communicating that portal registration is expected and is integral to the care process.”
— Josh Gray, Vice President, athenaResearch
1.3 Register patients in the office
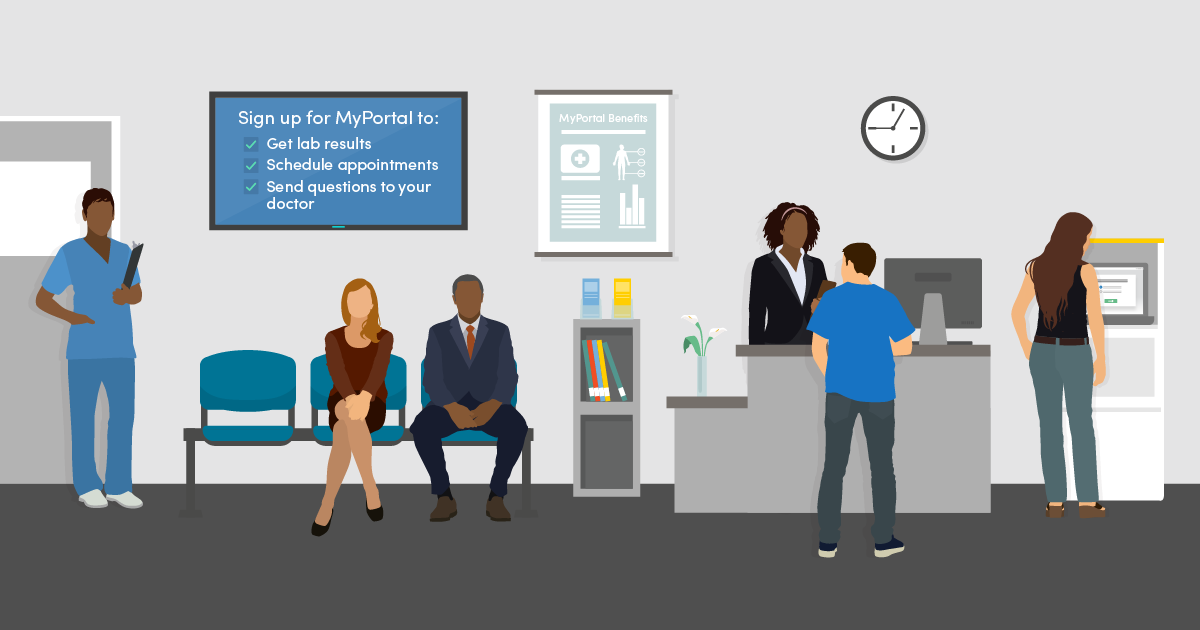
Treat patients’ office visits as a prime opportunity for portal registration.
Patients are more likely to register in the office, where they can get support from practice staff and engage in a personal conversation about benefits of the portal. If patients are asked to sign up once they’ve returned home, they may forget, have competing priorities, or struggle to navigate the technology on their own.
Make in-office registration the default by building it into your care delivery workflow and offering several registration touch points during a visit. For example, at check-in and check-out the receptionist, medical assistant, or nurse can teach patients about the portal and offer to sign them up on the spot using a kiosk, tablet, or registrar computer.
athenahealth 14 | From the field
athenahealth analyzed portal registration methods among 973,000 patients who visited practices that offer their patient portal, athenaCommunicator. athenahealth found in-office registration much more effective than at-home registration.
In-office registration
Among patients given the opportunity to sign up…

Using a kiosk or tablet, 57% signed up

On the registrar computer, 53% signed up

After receiving a text message, 23% signed up
At-home registration
Among patients who received…

An email at check-in, 12% signed up

An automated monthly email, 4% signed up

A marketing campaign invitation, less than 1% signed up
1.4 Market and educate effectively
Use positive, encouraging language — with both staff and patients — and leverage every educational opportunity.
Get staff buy-in
Strong leadership and staff buy-in to the patient portal can set the stage for effective marketing and lead to higher enrollment.
Tips for Practice Administrators 15
Practice leaders can take several steps to create an environment that encourages portal adoption.
- Provide opportunities for practice staff to discuss portal adoption, so that you can address fears and identify solutions
- Encourage staff to set up their own patient portal accounts, so that they can better understand the tool and its potential value to patients
- Offer staff incentives for portal adoption — for example, via practice-wide contests
- Promote the portal internally as a critical offering to patients, so that all staff view portal use as an opportunity for high-quality customer service
- Explain that it’s important for all clinicians to adopt the portal so that the practice can market consistently to all patients and avoid sending mixed messages
- Foster enthusiasm for the portal among staff, so that they can relay that enthusiasm to patients
Clinicians are key.
Individuals encouraged by their health care clinician to use their online medical record are almost twice as likely to access it compared to those who are not encouraged. In 2017, 63% of individuals who were encouraged by their doctor to use their online medical record accessed it within the past year compared to only 38% of those who were not encouraged. 16
Tell patients how they can benefit.
Ensure that all members of the care team can relay the benefits of the portal and show patients how to do basic tasks like view lab results, send messages, pay bills, and request or schedule an appointment. See Chapter 2 of this playbook for more information on portal benefits.
Give clinicians and staff talking points so that everyone reinforces the same key messages.
Consider jumping on board with the Blue Button Initiative, a public-private partnership to provide consumers with easy access to their health records in a format they can use. 17 The Blue Button symbol indicates to patients that they can download a personal medical summary that includes medications, conditions, and more. You can customize the Blue Button symbol to your practice.
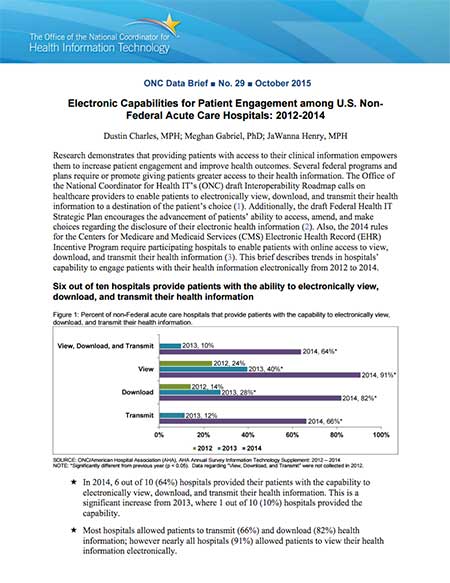
The Blue Button Initiative is having an impact
Between 2011 and 2014, the number of organizations participating in the campaign rose from 30 to 650. And in 2014, over half of patients offered access to their medical record online took advantage of the offer.
For more information on how patients’ access to their own data has grown, check out these ONC Data Briefs:
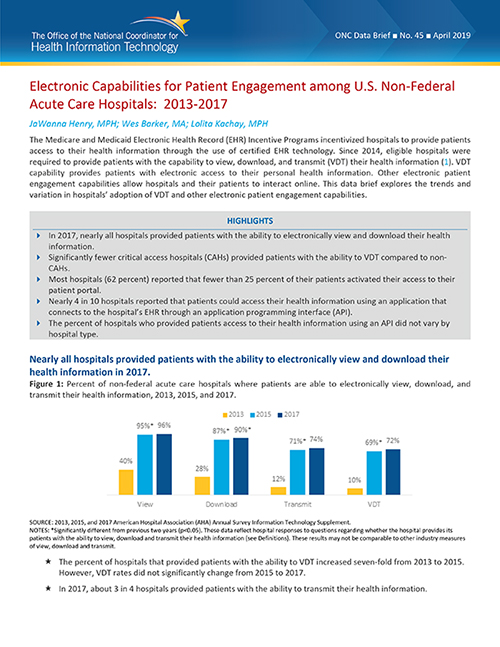
Electronic Capabilities for Patient Engagement among U.S. Non-Federal Acute Care Hospitals: 2013–2017 18
Take advantage of every touchpoint. 22
Take every opportunity to promote patient portal enrollment. Over the course of a visit, a patient may talk to several practice staff including a receptionist, nurse, and doctor. Treat each conversation with a patient as an opportunity to explain the portal’s value and highlight the simple steps patients can take to activate their account.
Use clear action steps!
Adding clear action steps to your after-visit summaries — with images in an appealing layout — may inspire patients to enroll in online portals.
You can also add portal enrollment steps to paperwork, such as after-visit summaries. Make the instructions actionable and easy for patients to understand — choose clear, direct language and use illustrations, bullets, and numbering where possible. Encourage them to take immediate action.
Adding clear action steps to your after-visit summaries — with images in an appealing layout — may inspire patients to enroll in online portals. It’s an affordable, scalable way to encourage patient participation.
Remember that marketing opportunities exist outside of a visit, too — like when patients call the office.
Tips for Practice Staff
Practice staff can take steps to make the most of each patient touch point.
- Teach patients about the portal while they’re waiting to see their doctors
- In the waiting room, have posters, brochures, and videos that highlight portal features. Ask your EHR vendor what materials they offer — many have developed portal marketing materials so that you don’t have to
- Give patients instructions for logging into the portal on a smartphone while they wait
- Set up a pre-recorded hold message or a message that plays at the end of a call that reminds patients to register
- Show patients the simple portal enrollment steps listed on their after-visit summary and encourage them to sign up
Make patient portal communication the norm.
Move away from traditional methods of patient communication, like phone and mail. Frame the patient portal as the best way to reach clinicians and see important medical information.
Inova Health | From the field
Inova Health partnered with ONC, the Office of Evaluation Sciences, and the Centers for Medicare and Medicaid Services to identify a solution to encourage patients to enroll in the health system's EHR patient portal. Working closely with its partners, Inova Health revised the after-visit summary (AVS) to make the benefits of EHRs salient, highlight clear action steps, and encourage immediate action. Analysis suggests that the revised instructions led to a 10% increase in the probability of online patient portal activation.
There are promising signs that clear action steps presented using images, and in an appealing layout, may encourage patients to access the online patient portal component of their health care system’s EHR. Read more about this low-cost and scalable solution to encourage patients to enroll and use portals.
Chapter 1 Recap
Take the first step toward patient engagement by facilitating easy portal enrollment.
- Choose a portal with a simple, secure signup
- Develop an automatic enrollment policy
- Register patients in the office
- Market and educate effectively
Chapter 2
Activate portal features that meet patient needs
In this chapter
Learn how to:
- Save time for patients and staff by enabling online booking and prescription refills
- Set up secure messaging to streamline patient-clinician communication
- Share notes to help patients understand and act on their clinician's advice
- Add value to the portal by including educational and community resources
- Create a user-friendly electronic records request process
Patient portals have the potential to streamline clinician workflow and improve patient engagement.
But at first, clinicians may be overwhelmed by the number of features that portals offer or fear that using the portal will be cumbersome and ineffective.
You can take small steps to overcome these barriers and get the most out of your patient portal. Although patient portals vary from vendor to vendor, most include a basic set of features that offer value to patients. These features can improve the way clinicians and patients:
- Handle administrative tasks, like booking appointments
- Communicate with each other
- Manage care
Use these features to engage your patients in their care and make care coordination and communication more convenient, efficient, and effective — for them and for you.
Keep in mind that other features may also be available — but make sure you’ve determined their value before adding them. If you clog the portal with unnecessary information and tools, patients may get overwhelmed and find the portal more difficult to navigate and use.
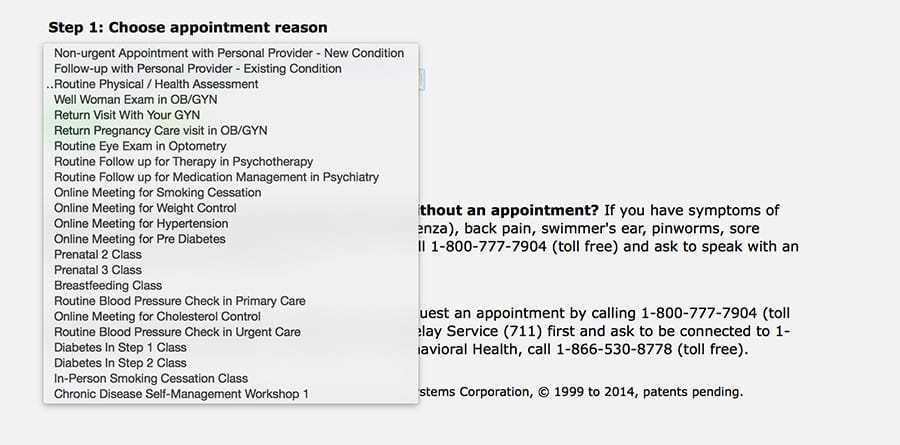
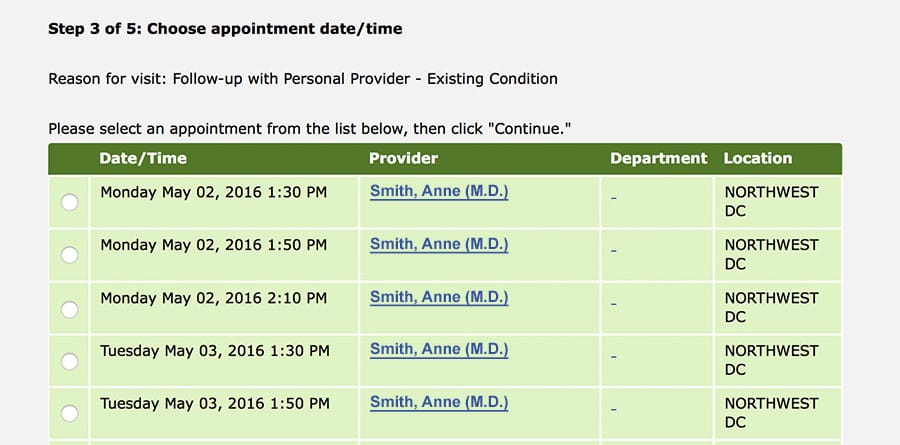
2.1 Enable online booking and prescription refills
Booking medical appointments and refilling prescriptions over the phone can be time-consuming for both patients and clinicians. On average, it takes a little more than 8 minutes to make an appointment over the phone. 23
In 2017, over half of non-federal acute care hospitals reported that they allow patients to schedule appointments and refill prescriptions through their portal. 24 Allowing patients to book medical appointments and refill prescriptions online will free up staff to support your practice in more valuable ways. 25 And research shows that patients use these features — in 2017, 39% of people with access to a portal used it to make appointments and 37% requested medication refills. 26
Kaiser Permanente | From the field
As of 2014, about half of Kaiser Permanente’s nearly 10 million members were using Kaiser’s online health management platform. In 2014, Kaiser members made more than 4 million online appointment requests and refilled more than 17 million prescriptions online. 27
Kaiser tells patients upfront when they can expect to get an appointment if they book online. 28
Through the portal, Kaiser also gives patients clear instructions for:
- Filling a prescription for the first time
- Refilling prescriptions online
- Transferring prescriptions from another health system
- Checking which medications are covered by their plan
- Reading up on medication instructions and side effects 29
2.2 Set up secure messaging
Between 2015 and 2017, the number of non-federal acute care hospitals that offered secure messaging through their patient portal increased by nearly 10%.30 By setting up secure messaging, your practice will take a big step toward achieving a Meaningful Use objective: “Use secure electronic messaging to communicate with patients on relevant health information.” 31
There are many scenarios in which patients and clinicians need to communicate between visits. Patients may have follow-up questions about a clinician’s guidance or a medication. 32 Clinicians may need to share test results or explain a recommendation in more detail.
Myth
Clinicians worry that activating email in the patient portal will lead to an email deluge that burdens their practice and impedes efficiency.
Reality
When practices integrate email into their workflow, clinicians often find communicating with patients more convenient and less time-consuming.
Using the portal, patients and clinicians can:
- Share brief messages and updates
- Clarify issues and advice
- Correct misunderstandings before they become significant problems
- Record details, like a referral name or post-operative instructions
- Link to educational materials and other online resources 33
Patient portals offer an opportunity to improve and streamline patient-clinician communication and practice workflow. The portal’s secure email can reduce the need for face-to-face visits and phone calls by giving patients and clinicians a quick, convenient way to exchange information.
With secure email through the portal, your practice can:
- Avoid telephone tag, which can lead to both miscommunication and communication delays
- Address routine health issues more efficiently, so you can dedicate more time to patients who need in-person care
- Have support staff to triage messages, so that clinicians only need to weigh in as necessary 34
- Share lab results — a best practice identified by some EHRs, like athenahealth — or other post-visit follow-up with patients
To maximize efficiency, practices must integrate reading and responding to email into their workflow. For example, assign a staff member to acknowledge all patient messages within 1 business day. Clinicians can then respond to the patient’s question or issue at their convenience. 35
Tips for Practice Administrators 36
If your practice uses the portal’s email feature, consider establishing policies that address:
- Turnaround time for responding to patient emails. Don’t use email for urgent issues.
- The types of communication allowed over email. Decide which requests (like prescription refills and appointment scheduling) clinicians will fulfill and which sensitive topics (like HIV and mental health) they’ll discuss.
Check out ONC’s Fact Sheet: Using Secure Electronic Messaging to Support Patient and Family Engagement.
Tips for Clinicians
Follow these guidelines for communicating with patients by email. 37
Address privacy issues
- Let patients know which other clinicians or practice staff may read and respond to their emails — for example, outside usual business hours or when you’re on vacation. Include this privacy disclaimer in each patient’s medical record.
- Keep a mailing list of patients, but only send group emails using the blind copy feature. Never send group emails where patients can see each other’s names.
Give patients clear guidance
Make sure to explain the policies and procedures for using portal email, like typical response time and types of communication allowed over email (see Tips for Practice Administrators above).
Also, ask patients to:
- Write a subject line that describes the nature of their email, like “Billing question” or “Medical advice”
- Call 911 or your office about urgent issues
For more information and guidance, check out ONC’s Fact Sheet: Using Secure Electronic Messaging to Support Patient and Family Engagement. 38
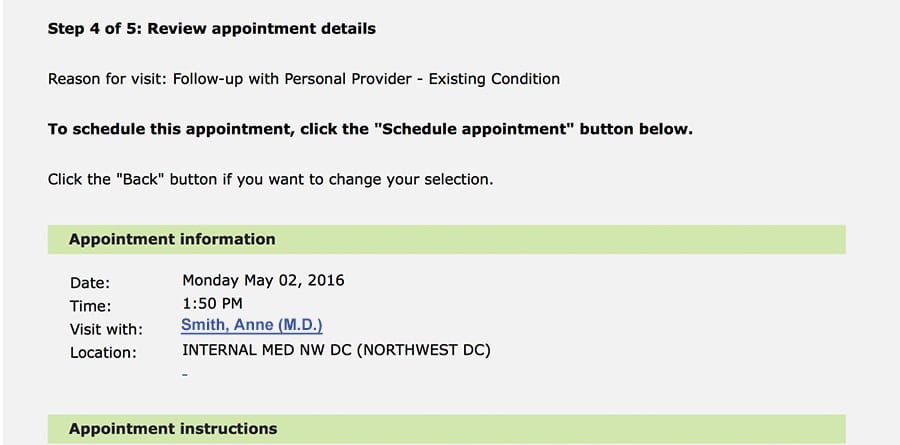
Kaiser Permanente | From the field
In 2014, Kaiser members used the portal to:
Lab test results and secure patient-clinician email became widely available to Kaiser Permanente members in 2006. Over the next year, the numbers of lab results viewed online and email messages sent to clinicians grew steadily. Between 2006 and 2007, lab test results viewed online increased 157% and email messages to clinicians increased 152%. Viewing test results soon became the most-used portal feature. 39
Kaiser members primarily emailed their clinicians to discuss:
- A change in health condition
- Lab results
- New condition
- Prescription dose
- The need for a new prescription
These emails can prompt necessary care that may have otherwise been overlooked. Six out of 10 patient-initiated emails led to new clinical assessments or decisions, and 1 in 4 required clinical action (like a lab test). 40
Primary Health Medical Group 41 | From the field
Primary Health Medical Group clinicians can send lab results to patients using secure messaging. Clinicians can include a brief message explaining the results (for example, “Your results are normal”) and any needed follow‐up instructions (for example, “Come back in 3 months for a recheck”). For serious lab results, clinicians use the phone to discuss results with the patient. Clinicians encourage patients to review their medical information and report inaccuracies.
2.3 Share notes
Patients immediately forget up to 80% of the clinical information they receive during a visit. 42 Clinician notes can give patients a snapshot of a visit so they can better remember, understand, and act on their clinician’s advice after the visit has ended. Patients have always had a right to see these notes — but until recently there hasn’t been a simple, straightforward way to access them. 43
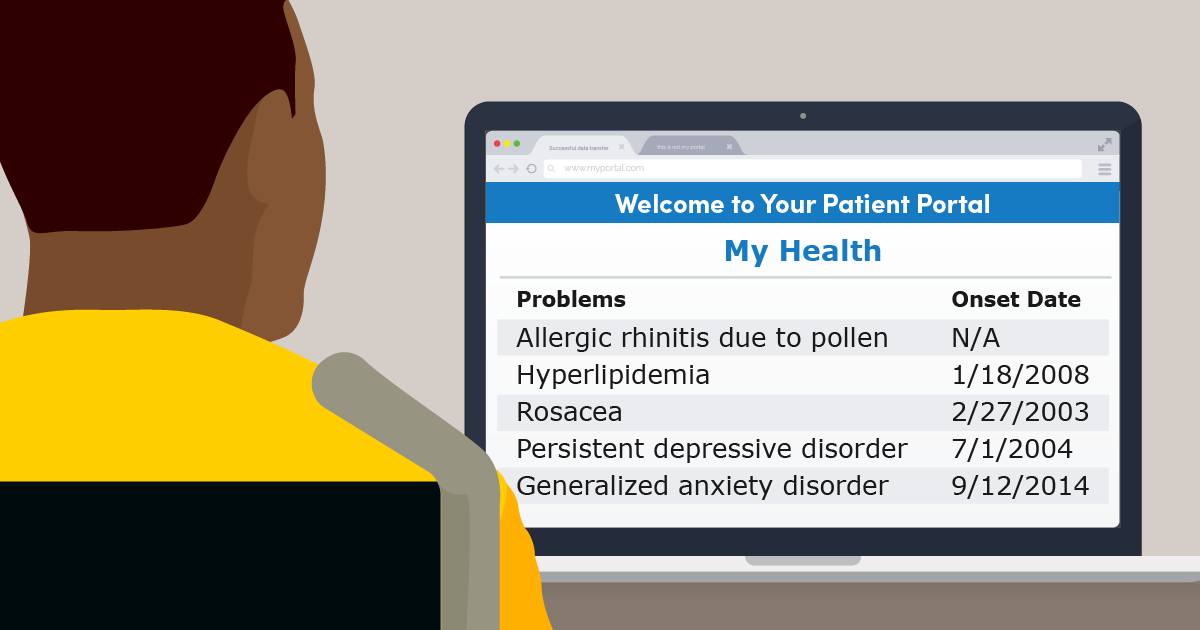
By offering patients access to notes through a portal, you can promote transparency and change the way people engage with their health and care. 44 Since patients are the best source of information about their health, they can also act as a second pair of eyes on the record. With patients checking for accuracy, clinicians can improve the quality of a medical record and make more informed clinical decisions. 45
Tips for Clinicians
When sharing notes with patients, it’s important to:
- Explain to patients what they can expect to see in the notes
- Use plain language instead of medical jargon or abbreviations
- Soften language and add context, when necessary (for example, instead of labeling a patient as “obese,” include their BMI and link to patient education about BMI)
- Keep notes focused on specific issues
- Discuss lab or study results, if applicable
- Reference educational materials, whenever possible 46
An Evaluation of OpenNotes 47 | From the field
A study across 3 sites — Beth Israel Deaconess Medical Center (BIDMC) in Massachusetts, Geisinger Health System (GHS) in Pennsylvania, and Harborview Medical Center (HMC) in Washington — found that most clinicians had positive or neutral experiences with OpenNotes (a national initiative that promotes sharing notes with patients 48 ). When asked about the most difficult aspect of OpenNotes, 3 out of 4 clinicians commented that nothing was difficult and that they experienced no changes in their practice. Several doctors acknowledged fears about an additional time burden and offending or worrying patients — but said that these concerns didn’t materialize.
The majority of patients who participated in the study used OpenNotes. Out of roughly 13,500 patients with access to clinician notes, more than 11,000 had opened at least 1 note.
Myth
Clinicians fear that patients may misinterpret or misunderstand their notes — causing more worry for patients and more work for clinicians.
Reality
For most clinicians, sharing notes doesn’t affect their workload — and using OpenNotes improves patients’ engagement and sense of ownership over their care.
Patients across all health systems reported experiencing benefits from seeing notes. Specifically:
77% to 87% across the 3 sites reported that OpenNotes helped them feel more in control of their care.
60% to 78% of those taking medications reported increased medication adherence.
20% to 42% reported sharing notes with others.
“Making visit notes available online is a good idea.”
— 85% to 88% of clinicians in the study agreed
Adopting OpenNotes: Partnering with Patients
OpenNotes isn’t software or a product — it’s an approach to giving patients access to notes from their health care visits. OpenNotes can benefit health care practices and patients by increasing transparency and patient engagement. Complete this module to learn 6 steps for adopting OpenNotes in your practice.
Go to the AMA STEPS Forward™ Adopting OpenNotes: Partnering with Patients module.
OpenNotes at Kaiser Permanente 49 | From the field
Kaiser has found that most patients with access to visit notes read them, and many discuss them with clinicians or loved ones. The majority of Kaiser patients who used OpenNotes reported improved self-care:
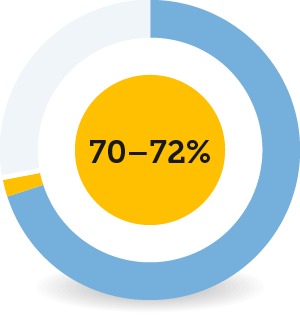
70–72% of patients reported taking better care of themselves.
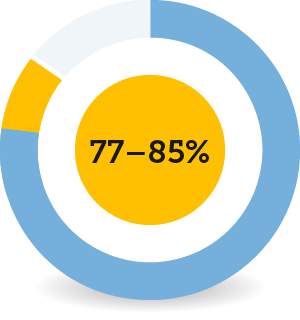
77–85% reported better understanding of their health and medical conditions.
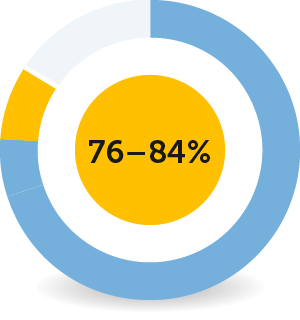
76–84% reported remembering to plan for their care better.

69–80% felt better prepared for visits.

77–87% felt more in control of their care.
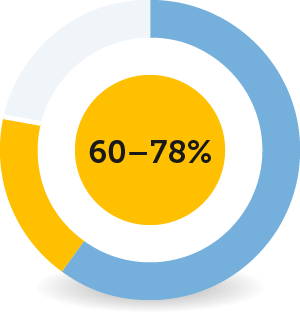
60–78% of patients taking medications reported improvements in taking medications as prescribed.
This increased patient involvement in health and medical care can lead to more efficient care, better patient-clinician communication and, ultimately, healthier outcomes.
Access to OpenNotes is important to the majority of Kaiser members: Roughly 6 of 10 members who logged onto KP.org after a recent visit said that OpenNotes would be a “very important” factor in future health plan decisions. About 4 of 10 who hadn’t logged on said the same.
“Reviewing the notes I SEE why I need to lose weight…It feels like my [d]octor really cares about my health, I never knew that.”
— Patient in study
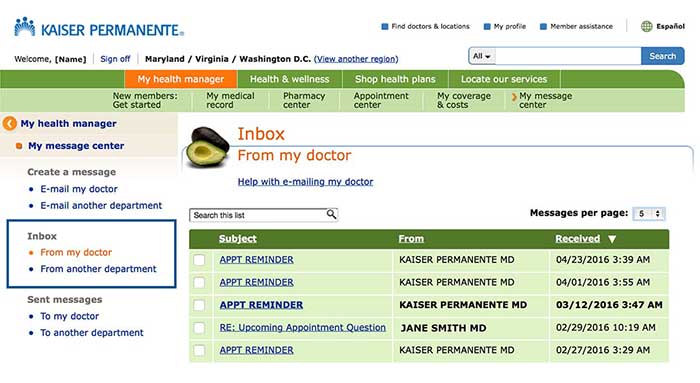
2.4 Connect your patients to educational and community resources
Research shows that adding educational resources to patient portals can make them more useful and effective 50 — and help you increase patient engagement. Portals and electronic health records can also help your staff provide tailored information and community resources to patients who may benefit from them.
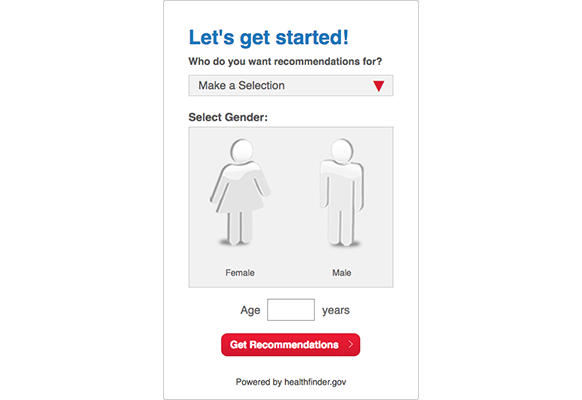
Try this tool!
Add the myhealthfinder tool to your portal or website.
When choosing educational resources to add your patient portal, it’s important to select trusted sources. For example, healthfinder.gov offers actionable, evidence-based, plain language health and wellness information, as well as free interactive tools like myhealthfinder, which provides personalized preventive health care services recommendations.
Because healthfinder.gov manages the content, you can add the tool to a portal or website without having to worry about keeping the information relevant and up-to-date.
You can also use your EHR to track social determinants of health: the social, economic, and environmental conditions that can affect health and health outcomes. Including this information in your EHR can help your staff identify and address factors that may contribute to health complications, such as unsafe housing or lack of access to safe opportunities for physical activity.
See the PRAPARE Implementation and Action Toolkit for resources on how to set up your EHR to gather data on social determinants of health, and how to assess and respond to that data once it’s collected.
CommunityRx | From the field
To address key social determinants of health on Chicago’s South Side — like food access, employment, and social support — CommunityRx developed a real-time automated system called HealtheRx. The system connects patients to community-based services and resources that can help them stay healthy and manage chronic conditions.
HealtheRx is embedded in EHR systems and seamlessly integrates with clinic workflow, matching patient health information with relevant wellness programs and services located near their home. Patients can also talk to dedicated Information Specialists to get help navigating and understanding the resources available to them.
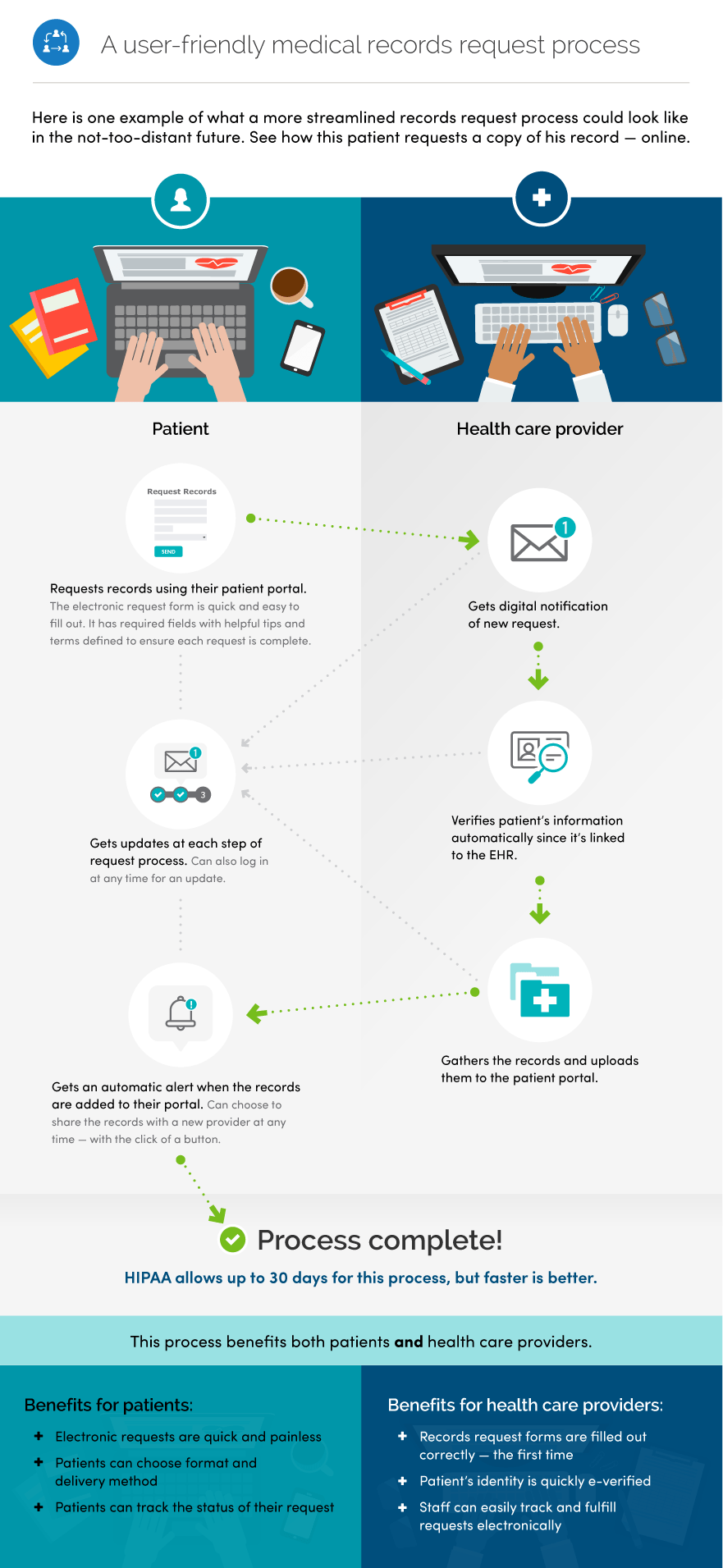
2.5 Support electronic records requests
More and more patient health information is available electronically — but patients and caregivers still face challenges in accessing, using, and sharing their data. Patient portals may not include all the information patients need — and what's there may be inaccurate or incomplete. And often, health data can’t be requested or shared electronically, or transferred to other health care clinicians without a cumbersome, multi-step request process.
To learn more about the challenges patients face in the records request process, check out ONC’s report Improving the Health Records Request Process for Patients: Insights from User Experience Research [PDF - 2.6 MB]. The report includes personas and journey maps illustrating these challenges, as well as tips on creating a better records request process.
We know that patients and caregivers who do have access to their data can better coordinate their health care, prevent repeat or unnecessary tests and procedures, and have greater control over their health and well-being.
That’s why ONC is committed to addressing large-scale access and portability issues — to help in creating a medical records request process that works for everyone.
There’s a lot that health care practices can do today to improve the records request process and reduce the burden on consumers, clinicians, and care teams. Integrating records requests into your patient portal is a win-win — it increases patient satisfaction, saves time, and reduces hassle for clinicians, administrators, and other practice staff.
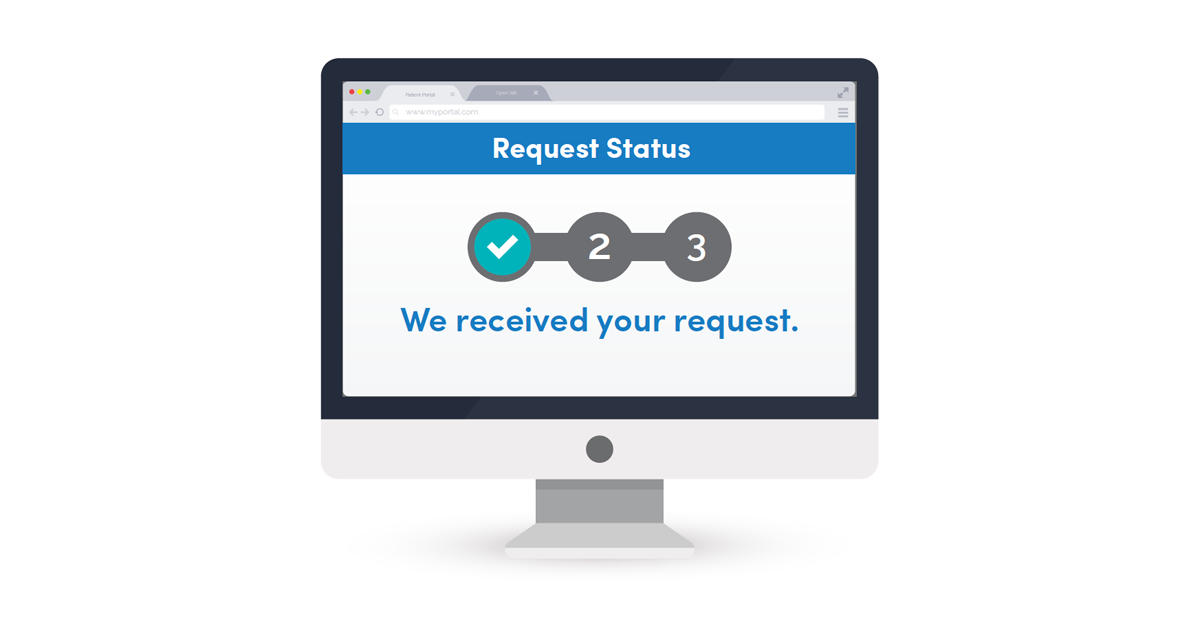
Health Records Request Wizard | From the field
The Health Records Request Wizard is a new tool designed to make it easier for patients to request their health records. The wizard was created by a group of health care organizations, including X4Health and Swellbox. It's currently in the prototype phase.
The Request Wizard asks the patient a series of questions, using the answers to populate a HIPAA-compliant digital PDF request form. By asking about patients' needs upfront, the Request Wizard can create a form that only requests the specific information that is needed, such as vaccination records, notes from a particular surgery, or a full medical record.
This innovative tool is designed to make the record request process painless for all involved. It offers patients a simple, streamlined experience when requesting their health records — and it helps practices save time and resources that would otherwise be spent explaining the process to patients.
Novant Health | From the field
Novant Health, a network of clinics and hospitals headquartered in North Carolina, makes it easy for patients to request health records electronically. The Novant Health website offers clear instructions for submitting a medical records request, including answers to frequently asked questions about the process.
Novant Health patients can request medical records:
- By fax
- By email
- Via their patient portal
Allowing patients to submit a record request electronically is a great way to increase patient access. With both email and patient portal submission as options, patients can submit their request at a time that’s convenient for them — instead of having to locate a fax machine or hand-deliver a request form during office hours.
Using the patient portal as a tool to access medical records also enables patients to request and view their health data on their own time. The portal verifies patients’ identity through the login, and the electronic request form is easy to fill out and secure to submit.
Chapter 2 Recap
Take advantage of patient portal features to improve communication and create value for patients and clinicians.
- Allow online booking and prescription refills
- Set up secure messaging
- Share notes
- Connect your patients to educational and community resources
- Support electronic records requests
Content last updated on: May 31, 2019
Chapter 3
Ensure all patients can access and understand information
In this chapter
Learn how to:
- Take steps to ensure your portal is accessible for all patients
- Address privacy concerns related to adolescents’ health information
- Create materials to support non-English-speaking patients
Patient portals can be a powerful force in patient engagement — but it’s important for them to be inclusive and accessible. In 2017, nearly 1 in 5 individuals who were offered access to their online medical record but didn’t view it said they didn’t have a way to access the website.51
Depending on your patient population, trouble accessing or using the patient portal can contribute to health disparities — preventable differences in health outcomes between groups of people that are closely linked with social, economic, or environmental disadvantages. For example, if a portal’s medication refill reminders are only available in English, patients with limited English proficiency may be less likely to get the medications they need to manage chronic conditions.
When setting up your portal, take steps to ensure that it meets the needs of all your patients.
3.1 Ensure portal access for all patients
To support all patients in accessing their health information, you can:
- Offer your patient portal in multiple languages
- Make sure your portal is mobile-friendly, and that the pages load quickly, so that users with limited data or slow connections can still access it
- Check that your portal is easy to navigate for patients who use screen readers or other assistive technology
You can also include information that helps your staff provide culturally and linguistically appropriate care — for example, data fields indicating patients’ gender pronouns and whether they prefer to be addressed by first or last name.
Make your patient portal accessible to caregivers, too.
For patients who are unable to access or use their portal (due to factors like limited cognitive function, lack of education, or inexperience with technology), family members or friends are essential members of the care team.52
Take steps to allow portal access for caregivers while accounting for the diverse roles caregivers can play and patients’ varied needs and desires.
The NewYork-Presbyterian Portal Help Desk | From the field
NewYork-Presbyterian (NYP), a health care delivery system in New York City, has implemented a support service to help patients overcome common challenges to using their patient portal. After launching the MyNYP patient portal in 2009, NYP looked for ways to help patients make the most of it. In 2012, the organization launched a portal Help Desk [PDF - 414 KB] to provide added support for portal users.
Four full-time staff who speak English, Spanish, and Chinese run the Help Desk, fielding 120 to 160 requests each week. They solve technological issues and also help patients who struggle with finding information on the portal. They are able to track and respond to requests online, and they can address common errors in a patient’s information.
To ensure the Help Desk’s efficiency, NYP established clear standards for responding to requests. Staff members typically respond to patients’ online requests in 1 to 2 business days — and they make every effort to resolve the issue at first contact by working with other hospital departments and facilities as needed, rather than referring patients elsewhere. For example, if a patient is looking for information that typically isn’t available on the portal (like certain sensitive health information), the Help Desk works with the Medical Records department to upload that data to the patient’s record free of charge.
After NYP updated some features of their portal, the Help Desk saw the complexity of requests increase while the total number of requests went down. This indicates that NYP has increased patient engagement by offering additional, comprehensive portal services.
3.2 Address adolescent health and privacy concerns
For adolescent patients (ages 12 to 17), setting up varied levels of access can be particularly tricky. Adolescents may want to keep their health care decisions and medical information private, but laws vary from state to state.
Some state laws allow minors to receive specific kinds of health care, like mental or sexual health services, without their parents knowing or consenting. Others say that minors can make decisions on their own if they have an “adult status,” like being married or in the military.53
Parents may also want to keep certain information, like a family history of disease, between only themselves and their adolescent’s provider.
Boston Children’s Hospital54 | From the field
Boston Children’s Hospital (BCH) advocates for patient portals with flexible access that providers can tailor to meet patients’ and parents’ needs and to comply with relevant federal and state law.
Specifically, BCH recommends a portal that gives adolescents and parents access to different types of information. Following this model:
- Adolescents can see nearly all of their medical information, including anything sensitive — like a birth control pill prescription or chlamydia test results. They can’t see any information that their parents have asked to keep private.
- Parents can see information they’ve shared with their adolescent’s provider and general information about their adolescent’s health.
Adolescent MyChart55 | From the field
The University of California at San Francisco (UCSF) has customized MyChart — the patient portal offered through their EHR vendor, Epic — to offer appropriate patient and representative access that meets Meaningful Use requirements. The result is Adolescent MyChart.
Adolescent MyChart gives each audience access to distinct portal information.
| Content | Parent Proxy 0-11 years |
Parent Proxy 12-17 years |
Adolescent 12-17 years |
|---|---|---|---|
| Labs | YES | SELECTED | SELECTED |
| Immunizations | YES | YES | YES |
| Allergies | YES | YES | YES |
| Growth Chart | YES | YES | YES |
| Messaging to and from provider * | YES | YES | YES |
| Appointment Request | YES | YES | YES |
| Appointment View | YES | NO | YES |
| Problem List/Summary | YES | NO | YES |
| Medications/refill request | YES | NO | YES |
| * Parent and teen can send private messages to the provider. | |||
At UCSF, parents have limited portal access to potentially sensitive information about their teen children. This lines up with California law, which allows teens between ages 12 and 17 years to keep care for medical needs like sexually transmitted disease testing, contraception, and pregnancy care private. For example, parents can’t access lab results from a pregnancy test or OB ultrasound.
Through Adolescent MyChart, UCSF can more successfully engage teens in their care while also protecting their privacy.
“We made the decision to give teens their own access, and to make them able to see their full record, because we think it’s the right thing to do and it’s where we see patient-centered health information technology going.”
— Dr. Carolyn Jasik, Assistant Professor of Pediatrics, UCSF
3.3 Engage non-English-speaking patients
As you’re developing and improving your patient portal, it’s important to be inclusive and accessible to non-English-speaking patients as much as possible.
Options for supporting non-English-speaking individuals in your patient population include:56
- Use the portal landing page to make materials available in languages spoken by your patients
- Enable your system to send text messages to patients in languages spoken by your patients, either as part of the portal or as a stand-alone functionality
- Let patients know they may send secure messages to their provider in their native language — if you have workflows developed to translate and respond to these messages
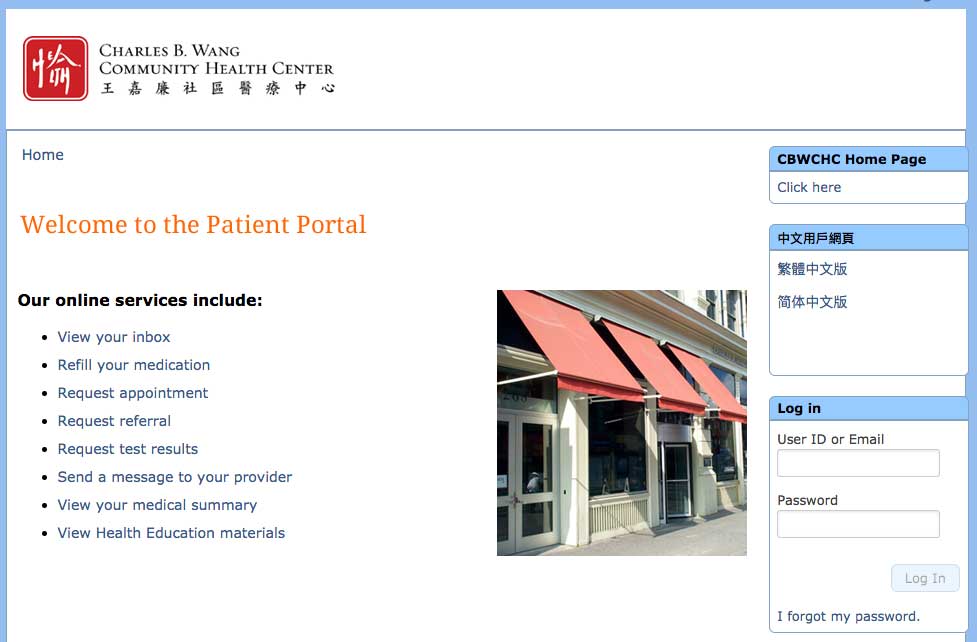
Charles B. Wang Community Health Center (CBWCHC) | From the field
Since December 2013, the CBWCHC Chinese language patient portal (CLPP) has provided services in Traditional and Simplified Chinese in addition to the Center’s original English platform.
Before launching the CLPP, an interdisciplinary project team collaborated to develop and review the portal, ensuring that it was easily accessible, culturally sensitive, and supportive of positive health outcomes.
“Promoting patient engagement through tools such as linguistically-appropriate patient portals is a key step for maintaining the importance of individual patient needs in receiving care services.”
— Lynn Sherman, MBA, Chief Financial Officer at the Charles B. Wang Community Health Center
Chapter 3 Recap
Look for opportunities to make your patient portal accessible and secure for all users.
- Take steps to ensure your portal is accessible for all patients
- Address adolescent health and privacy concerns in the context of relevant state laws
- Create materials to support non-English-speaking patients
Content last updated on: April 17, 2019
Chapter 4
Allow portal access for caregivers
In this chapter
Learn how to:
- Set up levels of access so patients and caregivers can see different information
- Help patients engage in advance care planning (ACP)
Allowing family members and caregivers to access patient health information through a portal is becoming much more common. In 2017, 86% of non-federal acute care hospitals reported offering this access to patients and their loved ones. 57
Despite this, clinicians and practice administrators often struggle to navigate federal and state laws related to proxy access (allowing someone other than the patient to see a patient’s health information). Laws like the Health Insurance Portability and Accountability Act (HIPAA) are designed to keep patients’ medical records and personal health information private and secure.
However, in some situations it is appropriate or necessary for a family member, friend, or other caregiver to have access to a patient’s health information so that they may coordinate, deliver, or oversee care.
Other examples of people who may need to access patient information include:
- A home health aide to a chronically ill patient
- A health care power of attorney responsible for an incapacitated patient’s medical decisions and care 59
Under HIPAA, a patient’s personal representative (someone authorized under state or other applicable law to act on behalf of the patient) has a right to access the patient’s personal health information. The patient also has a right to allow their personal representative to share this information with someone else, like a doctor or hospital. 60
The opportunities created by caregiver access to patient portals include: 61
Patient Success Story
Suzanne Mintz, caretaker
"Portals make you feel like you are a member of your own care team."
- Enabling providers to differentiate with whom they are exchanging secure messages: the patient or someone else involved in their care
- The ability to respect patient preferences for including others in their care
- Improved transitional care by providing family caregivers with timely, accurate, and comprehensive information after patients have been discharged from the hospital
- Greater collaboration between clinicians and family caregivers
- More impactful involvement of caregivers in patients’ self-management plans
- Greater information transparency, which enables family caregivers to alert clinicians to missing or inaccurate information in patients’ health records
Increasing shared access to patient portals by caregivers is the next step in patient engagement. It has the potential to increase clinical quality and patient safety, add to the convenience and timeliness of health system interactions, and strengthen partnerships between patients, caregivers, and clinicians.
Tips for Practice Administrators 62
Practice administrators can take steps to enable caregivers’ access.
- See if your EHR vendor allows providers to set varying levels of access to a patient’s portal information
- Work with your EHR vendor to make sure you can give each personal representative a unique, secure login to access the patient’s portal
- Make sure that staff and clinicians understand registration processes for granting shared/proxy access — and identify practice workflows for implementation
- Consider strategies to promote awareness about the availability of shared/proxy access among your patients, staff, and clinicians
Tips for Clinicians
Clinicians play an important role in managing caregivers’ access.
- Talk with your patient to find out who is involved in their care
- Ask about your patient’s preferences for giving caregivers access to their health information (HIPAA generally allows a provider to share health information with family members or friends involved in the patient’s care unless the patient objects) 63
- Customize caregivers’ access to your patient’s portal information, if possible
4.1 Set up varying levels of access
Many patient portals still offer a one-size-fits-all approach to information access where anyone with the right login can see the full medical record. Some patients share their own login credentials with their caregivers, but this gives caregivers unlimited access to the patient’s information — including being able to view private messages to or from clinicians.
An environmental scan of 20 large and geographically diverse health systems found that the majority of them give caregivers full access to patient portal information and features, yet the researchers also reported that patients’ preferences for sharing their health information with others involved in their care vary widely. The study indicates there’s still much to be done in both promoting awareness and differentiating levels of access that respect patients’ choice and control of their health information. 64
Establishing different levels of access can help you balance the competing needs of patient privacy and caregiver access. Giving caregivers their own unique login to your portal has other advantages beyond respecting patient privacy. It can also:
- Increase security by tracking the portal use of each individual, instead of a caregiver using a patient’s credentials 65
- Increase the amount of meaningful data available to learning health systems by capturing both patient-reported and caregiver-reported data 66
Tip for Practice Administrators
Allow patients and their representatives to see different information and access different features, depending on a patient’s needs and characteristics as well as relevant laws.
4.2 Integrate advance care planning documents
Try this tool!
Share the PREPARE website with your patients to help them with end-of-life planning.
End-of-life planning, or advance care planning (ACP), has been shown to increase patients’ satisfaction with their health care and improve quality of life for people with a terminal illness. 67 But completing and documenting this process can be challenging for both patients and clinicians.
Patient portals can help with advance care planning discussions and boost patient satisfaction. 68 If your portal includes an ACP feature, consider promoting it to your patients. In lieu of that, some systems include the ability for patients to securely upload documents. If that’s an option, invite patients to add a PDF copy of their plan to their electronic record.
Planning for End-of-Life Decisions with Your Patients
Patients and their families can benefit from making end-of-life decisions ahead of time. Training health practice staff on how to approach this sensitive topic can help patients feel more comfortable making these decisions. Complete this module to learn the 4 steps to helping patients prepare their end-of-life letter.
Go to the AMA STEPS Forward™ Planning for End-of-Life Decisions with Your Patients module.
Chapter 4 Recap
To help meet patient and caregiver needs:
- Set up varying levels of portal access
- Help patients engage in advance care planning
Content last updated on: May 31, 2019
Chapter 5
Integrate patient-generated health data and EHRs
In this chapter
Learn how to:
- Take steps to track patient-generated health data
- Improve preventive care by efficiently collecting family histories
Historically, clinicians have had limited access to data on patients’ health and well-being. They’ve made do with information collected during patient visits, like self-reported lifestyle habits and family health histories.
Technology is transforming our ability to collect accurate, reliable patient data.
In 2017,
More than
4 in 10
smartphone or tablet owners used their device to track progress on a health-related goal.69

Adults with chronic conditions are most likely to track health indicators, like blood pressure or symptoms, than those without.70
Using technology, patients can also share information that’s critical for health care decision-making but often too time-consuming or cumbersome for clinicians to gather — like family medical histories. What’s more, patients can provide this data from home, so that clinicians can maximize precious office visit time.
This chapter describes how you can use the patient portal to systematically collect patient-generated data and harness them to improve clinical care and patient health.
5.1 Track patient-generated health data
Across the nation, patients’ phones and computers are teeming with patient-generated health data: health-related data that patients create, record, or gather to help address a health concern. They include:
- Health history
- Treatment history
- Biometric data, like blood pressure readings
- Symptoms
- Lifestyle choices, like diet and exercise habits71, 72
As the amount of available data has grown, so too has our ability to collect, organize, and make sense of it all. More and more health systems are aggregating patient-generated health data in their EHRs and relying on these data to conduct remote monitoring — that is, to track patients’ wellness outside the clinic.
Clinicians can take advantage of these patient-generated health data to fill information gaps — and, ultimately, improve clinical decision-making, care delivery, and health outcomes.
The results are real for practices as well as patients:
- Fewer hospital readmissions, which can help avoid penalties for excessive readmission imposed by Centers for Medicare & Medicaid Services73
- Efficient diagnosis of illnesses, which saves practice resources
- Enhanced patient-centered care, so that clinicians can identify treatments and health behaviors that patients will follow through with
- Effective management of complex chronic conditions, so that patients can control their own health with less clinician intervention
“Using these tools — a wireless scale and bracelet-style activity tracker — my doctors and I have been able to assess intervention effectiveness, adjust dosages, unearth side effects, and clarify decision points.
Without the objective measure provided by my activity tracker, we would be basing our decision on my subjective assessments of getting worse… By putting my data to work for me, we can now do better.”
— Donna Cryer, liver transplant survivor74
Tips for Clinicians
Clinicians can use patient-generated health data to:
- Show how a patient is doing between visits
- Illustrate a patient’s health and behavior over time
- Inform strategies for preventive care and chronic disease management
- Improve patient safety by providing insight into medication adherence and allergies75
- Spark and support conversations with patients that result in shared decision making76
- Predict hospital readmission risk
Portals can streamline data collection by giving patients a platform for securely sharing information and completing online questionnaires. Clinicians can use the portal to send patients reminders to submit data and to follow up with patients as needed.
Tips for Practice Administrators
Consider taking steps to integrate patient-generated health data into your practice:
- Talk to staff about how patient-generated health data can improve care and efficiency
- Assess what data you’re already gathering and what additional data would be valuable
- Develop policies and procedures, like when to accept data and who will review them
- Educate patients and families about the value of and expectations for sharing patient-generated health data
- Start small — for example, by launching a pilot to collect symptoms for patients managing a chronic disease — and make changes as needed77
See HealthIT.gov for more information on patient-generated health data.
Patient-Generated Health Data Practical Guide
Overview
Document detailing best practices identified from 2 pilot demonstrations that tested concepts for the use of patient-generated health data in clinical care and research settings
Who it's for
Clinicians, researchers, health IT professionals, and health care administrators
When it's used
To learn suggested practices and questions to consider when implementing the capture, use, and sharing of patient-generated health data
Download the Patient-Generated Health Data Practical Guide [PDF - 392 KB]
Ochsner Health System78 | From the field
“In the past, we relied on patients to log information, bring it to us, and then we would input the data and decide a course of action. Now we can share information seamlessly between patient and physician to allow real-time, accurate analysis of a patient’s health status.”
— Robert Bober, MD, Director of Cardiac Molecular Imaging, Ochsner Medical Center
Ochsner Health System (OHS) is advancing the use of patient-generated health data through partnerships with Apple and its EHR developer.
Since October 2014, OHS has leveraged Apple HealthKit to create a more comprehensive picture of ongoing patient health. HealthKit, an iOS app, acts as a health dashboard by capturing health and activity data from other apps and wearable devices, like FitBit and Withings wireless blood pressure monitor.79, 80 Healthkit also has an open API (application programming interface), which enables other web applications to access its data. Using the API, OHS connected HealthKit to its EHR. As a result, OHS patients can automatically import HealthKit data into their EHRs and share it with clinicians.81
OHS piloted this integration in its Digital Medicine Program. The Digital Medicine Program, which focuses on patients with hypertension, uses remote monitoring to collect data including body weights and blood pressure measurements — all without patients leaving their homes. Clinicians and pharmacists see the data and follow up with patients in real time by, for example, adjusting their medications or tailoring lifestyle recommendations.82 One year in, OHS patients reported improved outcomes, engagement, and satisfaction with their care.
Among patients with uncontrolled blood pressure, 2 out of 3 had their blood pressure in control within 90 days of enrolling in the program.83 For patients, lower blood pressure means a lower likelihood of heart attack, stroke, and kidney failure — and greater peace of mind.
“For the first time in my life, I feel a sense of peace and comfort knowing that I’m under constant supervision and receiving high-quality care with little effort throughout my daily routine. This is the way health care should be.”
— Andres Rubiano, 54 year-old Digital Medicine Program patient who suffers from hypertension
Carolinas HealthCare System (CHS) launched a new mobile application for patients, called MyCarolinas Tracker, that uses an open API. That means CHS’s app can easily talk to other apps — allowing it to pull in health and fitness data from more than 100 devices and clinical data from clinicians. Patients can then use the app to track their wellness and clinical progress.
Patient-generated health data aren’t necessarily limited to patients’ phones. Patients can also use sensing devices, like blood pressure cuffs and pulse oximeters, to wirelessly share clinical information with clinicians.
The Center for Connected Health (CCH) implements programs rooted in connected health, a care model that uses information and communications technology — like mobile phones, computers, and wearable devices — to support patients’ health without disrupting their day-to-day lives.
CCCP cut heart failure-related hospital readmissions in half.
CCH’s Connected Cardiac Care Program (CCCP) showcases this approach. CCCP aims to improve self-management in heart failure patients at risk for hospitalization by combining:
- Regular clinical care
- Patient education
- Remote monitoring of indicators like blood pressure, heart rate, and weight
- Timely care and clinical feedback88
Clinicians used a central database to track all patient data. Data were also captured in patients’ EHRs.89
CCH conducted a retrospective study that evaluated the 4-month program90. At the outset, patients in the intervention and control groups had similar hospitalization rates. But for the duration of the program and up to 3 months after, hospitalization dropped significantly for patients enrolled in CCCP compared to those receiving typical care. CCCP patients also experienced significantly lower mortality rates during the program and for up to 4 months after discharge.91, 92
In addition to clinical outcomes, CCCP improved patients’ understanding of heart failure and self-management skills.93 These skills suggest a long-term payoff — even if patients have limited time in the program, they can still expect benefits down the line.
Clinicians come out on top, too. Even though CCCP costs $1,500 per patient, clinicians ultimately save $8,155 per patient from reductions in hospitalizations.94
“With our hospitals liable for thirty-day readmissions through CMS penalties, such interventions are becoming mainstay in the management of high risk patients.
As health technologies become more accessible and commoditized, programs like Connected Cardiac Care will be more affordable, and achieve an obvious return on investment.”
— Joseph C. Kvedar, MD, Vice President, Connected Health, Partners HealthCare
5.2 Collect family histories
“My goal over the past year has been to have the family history for most of my patients completed at least involving all first degree relatives. I did not find that this caused extra work or took much extra time – in fact it saved time and provided me valuable information for my practice.”
— Dr. Bruce Peyser, Medical Director, Pickett Road Clinic
Family health history can help predict a patient’s disease risk — essentially, it’s the simplest and least expensive form of genetic assessment.95 Traditionally, collecting and analyzing this information hasn’t been a routine part of primary care because of challenges like patients’ lack of knowledge about family history and clinicians’ limited time.
Now, technology-driven tools are changing the standard of risk assessments. These tools enable patients to systematically collect family health histories and report back to their clinicians. Clinicians can then ensure high-risk patients get necessary screenings and specialist care.96
Tips for Practice Administrators
To collect family histories efficiently and effectively, consider taking these steps:
- Encourage patients to enter pertinent family history through the patient portal — so they don’t have to recall family details during the visit
- Ask medical assistants to review family history before a visit — so clinicians don’t waste valuable visit time collecting that information
- Conduct clinical training about how to recognize genetic diseases and manage high-risk patients97
MeTree98 | From the field
The Genomedical Connection — a consortium between Duke University, the University of North Carolina at Greensboro, and the Moses Cone Health System in Greensboro, North Carolina — developed MeTree, a computerized self-administered family health history collection tool.
MeTree helps individuals have challenging conversations with loved ones about family health histories. It supports patients in collecting 3 generations of information on 48 conditions, including 20 cancers. The tool also generates a report for clinicians and patient-clinician talking points.
Clinicians can assess MeTree effectiveness by tracking appropriate screenings (like those for breast, colon, and ovarian cancers), testing for hereditary thrombophilia, and referrals to genetic counseling.99
By leveraging Fast Health Interoperability Resources (FHIR) — a new standard for exchanging health care information electronically100 — MeTree will soon connect to patients’ EHRs and allow patients and clinicians to seamlessly access this information.101
Chapter 5 Recap
Improve clinical decision-making by leveraging technologies to:
- Track patient-generated health data
- Collect family histories
Content last updated on: May 30, 2018
Chapter 6
Leverage APIs and other health IT
In this chapter
Learn how to:
- Use APIs to help patients access their data and take an active role in their health
- Evaluate health apps to use as tools for patient engagement
mHealth — the use of mobile and wireless technologies to promote health — is an ever-changing field with great potential for patient engagement.
There are a growing number of patient-facing mobile applications and online tools designed to give patients access to their health information. These tools and apps can help people:
- Effectively manage chronic conditions
- Participate in research
- Share data with clinicians in real time
- Take a more active role in their health care
There are also numerous apps to help patients manage specific health conditions like diabetes or epilepsy.
6.1 Use APIs to help patients control their data
One way for patients to access their EHR data is through an Application Programming Interface (API). The availability of APIs enables third-party app developers to connect patients' EHR data to new types of applications and online tools.
By enabling third-party API access to data from your EHR when patients request it, you can help empower your patients to use these innovative tools to support their health goals.
Yale Center for Clinical Investigation/Hugo | From the field
Yale Center for Clinical Investigation (YCCI) is collaborating with HUGO, a health data platform which gives patients seamless access to their electronic medical record — as well as data from other health systems and wearables or other devices — through the use of APIs.

Hugo app
Patients in the YCCI studies can use the Hugo app to aggregate their data from many types of EHRs. This puts patients in control of their data, allowing them to easily review their medical history, become partners in clinical research, and engage with researchers by responding to simple surveys via secure transmissions.
“We are just now scratching the surface of what will be possible with Hugo and this kind of patient empowerment. By enabling people to be active partners in research, we are accelerating progress towards a new generation of breakthroughs and a 21st century learning health system.”
— Allen L. Hsiao, MD, Chief Medical Information Officer, Yale School of Medicine & Yale New Haven Health
6.2 Use apps to support patient engagement
It’s no secret that mobile phones are everywhere these days, since 95% of Americans now own a cellphone of some kind — and 77% own a smartphone.102 The options for health apps are numerous, ranging from activity trackers to medication reminders and chronic condition self-management tools.
A 2013 study found that 9 in 10 patients would use an app if their doctor prescribed it.103 It also found that people who use mHealth tools are more likely to follow their clinicians’ advice and to be proactive about their health care.104
However, we still have a lot to learn about which “prescribable” apps are most effective.105 As more health professionals try out these new tools, the amount of information about the best ways to develop and use apps for patient engagement is sure to grow.
Evaluate and pilot test apps before recommending them
If you’re thinking of recommending an app for patient engagement — whether related to general wellness or for managing a specific health challenge — it’s important to do your homework. The following steps will help you evaluate whether an app is user friendly and appropriate for your patients.106
- Review the literature: Search the scientific literature for app reviews and clinical trials
- Search app clearinghouses: Websites that review apps can help you identify pros and cons of specific apps
- Search app stores: Be sure to use specific key words, including terms related to the health condition or target behavior
- Read user ratings and reviews: Look for positive comments about how the app works, how easy it is to use, and how effective it is
- Read the privacy notice: Make sure that the app will protect your patients' health information by checking out the app's privacy notice
- Ask your professional and patient networks: Use social media to find out what apps people like or are interested in
- Pilot test the app: Try it out yourself — or enlist a helper — to assess the app’s functionality, accuracy, and usability
- Get patient input: Once your patients have tried the app, don’t just talk about their health data — ask them how they like the app, too
There’s a lot to consider when researching and pilot testing an app! Of course, ease of use is key — but quality and safety are also essential.
- Usability is the “effectiveness, efficiency, and satisfaction with which specific users can achieve a specific set of tasks in a particular environment.” To learn more, check out Selecting a Mobile App: Evaluating the Usability of Medical Applications.
- Some factors that affect the quality and safety of a health app depend on the type of information or health condition the app addresses. Developing a Framework for Evaluating the Patient Engagement, Quality, and Safety of Mobile Health Applications lists some of the factors to consider.

Chapter 6 Recap
Improve clinical decision-making by leveraging technologies to:
- Use APIs to help patients access their data and take an active role in their health
- Use apps to support patient engagement
Content last updated on: May 31, 2019
Chapter 7
Improve appointments with health IT
In this chapter
Learn how to:
- Engage patients with their notes during visits
- Keep visits patient-centered while using EHRs
- Set up for live video appointments
A good relationship between patients and their health care team is a key part of successful care — and it’s influenced by many factors. As health IT continues to evolve, new opportunities and evidence are emerging about how EHRs and other health IT can strengthen patient-clinician interactions.
7.1 Build trust with patients through visit notes
There are many benefits to allowing patients to access visit notes through their patient portal. One benefit is a better, more trusting relationship between patients and clinicians. Sharing notes has been shown to improve the patient-doctor relationship, especially for patients of color, patients with poorer self-reported health, and patients with less education.107
An innovative way to engage patients with their EHR is to have a dual-screen setup where the patient can see what the clinician is typing during the appointment. A preliminary study found 100% patient satisfaction with this approach.108
Another option — especially for patients who may have barriers to accessing their portal from home — is to print notes out for them at the office.
7.2 Balance technology with interpersonal communication
As we’ve established, the potential upside of health IT is huge — that’s what this playbook is all about! But it’s also hard to overstate the value of good, old fashioned eye contact and other nonverbal cues for building trust and rapport with patients during their time in your office.
While evidence shows that EHRs can make patient visits more complicated, there are also opportunities to make visits more patient-centered.109 When you’re seeing patients, be sure to spend a portion of the appointment looking at them instead of your computer as you talk — and tell them what you’re doing as you use their EHR.
You can also take the opportunity to confirm that the information in your patient’s EHR is correct. Asking patients to validate their information with you in the room is another way to foster the patient-clinician relationship.
Optimizing Space in Medical Practices
The design and arrangement of clinic space affects how physicians and patients interact. Simple changes can enhance workflows, patient safety, and patient and team satisfaction. Complete this module to learn quick, cost-effective ways to improve your practice’s exam rooms and team areas.
Go to the AMA STEPS Forward™ Optimizing Space in Medical Practices module.
Listening with Empathy
When clinicians practice empathetic listening, patients report higher levels of satisfaction. Complete this module to learn the 8 steps to listening with empathy. You’ll also learn about tools and resources that can help you and your team master empathetic listening.
7.3 Offer video appointments
With telemedicine, technology lets clinicians provide some types of care to patients remotely.110 Telemedicine — specifically, video appointments — offers several advantages. These include:
- Improved access to care for patients, especially those in rural areas111
- Higher patient satisfaction112
- Lower out-of-pocket costs for patients113
- Improved management of chronic conditions114
If your practice plans to offer telemedicine, learn more about it in the Health IT Playbook.
Take steps to optimize video appointments
For clinicians who provide live video appointments with patients, these basic pieces of set-up and etiquette can make the interaction smoother and more engaging for your patients:115
- Make sure you have good lighting and aren’t lit from behind
- Know how to quickly mute yourself in case there’s background noise
- Be careful doing things like shuffling paper or typing when your microphone is on
- Have a simple background without doors, windows, or other distractions
- Angle the camera so you can make eye contact with your patients
Keep in mind that telemedicine may be a new experience for your patients, and walk them through the process so they know what to expect. For example, if you have to look away to write down notes, say what you’re doing.
Chapter 7 Recap
Use health IT to improve care and engage patients in innovative ways.
- Allow patients to see their notes during appointments
- Make sure technology supports — but doesn’t take over — in-person appointments
- Follow best practices for video appointments
Content last updated on: April 17, 2019
References
Introduction
1Gruessner, V. (n.d.) Three Vendors are Driving Patient Engagement and Portal Use. EHR Intelligence. Retrieved from https://ehrintelligence.com/news/three-vendors-are-driving-patient-engagement-and-portal-use
2Black Book Research (2018, April 20). Hospital Technology is the New Determiner of Patient Satisfaction, 2018 Black Book EHR User Survey Results. PR Newswire. Retrieved from https://www.prnewswire.com/news-releases/hospital-technology-is-the-new-determiner-of-patient-satisfaction-2018-black-book-ehr-user-survey-results-300633556.html
3Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
4 The long awaited end of meaningful use. Definitive Healthcare. (2016, January 19). Retrieved from http://www.definitivehc.com/hospital-information-technology/medicare-meaningful-use-program?source=newsltr-blog&utm_source=newsletter&utm_medium=email&utm_campaign=02-02-16
5 EHR Incentives & Certification: Meaningful use definition & objectives. (2015, February 6). Retrieved from https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives
6 Emont, S. (2011, May). Measuring the impact of patient portals: what the literature tells us. Retrieved from https://www.chcf.org/wp-content/uploads/2017/12/PDF-MeasuringImpactPatientPortals.pdf [PDF – 610KB]
7 Patient access to online health action plans enhances rate of preventive care. (2016, February 9). Retrieved from http://share.kaiserpermanente.org/article/patient-access-to-online-health-action-plans-enhances-rate-of-preventive-care/; http://www.ajpmonline.org/article/S0749-3797%2815%2900780-1/abstract
8 Emont, S. (2011, May). Measuring the impact of patient portals: what the literature tells us. Retrieved from https://www.chcf.org/wp-content/uploads/2017/12/PDF-MeasuringImpactPatientPortals.pdf [PDF – 610KB]
Chapter 1
9 Goel, M.S.; Brown, T.L.; Williams, A.; Cooper, A.J.; Baker, D.W. (2011). Patient-reported barriers to enrolling in a patient portal. Journal of the American Medical Informatics Association, 18(1), i8-i12. doi: 10.1136. Retrieved from https://academic.oup.com/jamia/article/18/Supplement_1/i8/798747?searchresult=1
10 Clain, D. (2015, July 30). athenaResearch Study: the current state of patient portal adoption. Retrieved from http://www.athenahealth.com/blog/2015/07/30/athenaresearch-study-the-current-state-of-patient-portal-adoption
11 Siddhanti, R. Mana Health. (Personal communication, 2016, February 11).
12 ManaPortal signup process and screenshots: Siddhanti, R. Mana Health. (Personal communication, 2016, February 19).
13 Friedman, R. (2015, August 3). How practices get patients to use their portals. Call-out box Retrieved from https://www.advisory.com/research/medical-group-strategy-council/practice-notes/2015/august/what-we-know-about-portal-adoption-part-2
14 Clain, D. (2015, July 30). athenaResearch Study: the current state of patient portal adoption. Retrieved from http://www.athenahealth.com/blog/2015/07/30/athenaresearch-study-the-current-state-of-patient-portal-adoption
15 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3041333/
16 Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
17 About Blue Button. Retrieved from https://www.healthit.gov/patients-families/blue-button/about-blue-button
18 Henry, J.; Barker, W.; Kachay, L. Electronic Capabilities for Patient Engagement among U.S. Non-Federal Acute Care Hospitals: 2013-2017. (No. 45, April 2019). Retrieved from: https://www.healthit.gov/sites/default/files/page/2019-04/AHApatientengagement.pdf [443 KB]
19 Henry, J.; Pylypchuk, Y.; Patel, V. Electronic Capabilities for Patient Engagement among U.S. Non-Federal Acute Care Hospitals: 2012–2015. (No. 38, September 2016). Retrieved from http://dashboard.healthit.gov/evaluations/data-briefs/hospitals-patient-engagement-electronic-capabilities-2015.php
20 Patel, V.; Barker, W.; Siminerio, E. Trends in Consumer Access and Use of Electronic Health Information. (No. 30, October 2015). Retrieved from https://www.healthit.gov/sites/default/files/briefs/oncdatabrief30_accesstrends_.pdf [PDF - 2.1 MB]
21 Charles, D.; Gabriel, M.; Henry, J. Electronic Capabilities for Patient Engagement among U.S. Non-Federal Acute Care Hospitals: 2012–2014 (No. 29, October 2015). Retrieved from https://www.healthit.gov/sites/default/files/briefs/oncdatabrief29_patientengagement.pdf [PDF - 1.9 MB]
22 Strategies for improving patient engagement through health IT. Retrieved from https://www.healthit.gov/sites/default/files/final_vdt_sect_508_tested.pdf [PDF – 2.6MB]
Chapter 2
23 DelVecchio, A. (2014, December 16). Expansion of online appointment scheduling could lead to cost savings. Retrieved from https://www.healthit.gov/sites/default/files/page/2019-04/AHApatientengagement.pdf.
24 Henry J, Barker W, & Kachay L. (April 2019). Electronic capabilities for patient engagement among U.S. non-federal cute care hospitals: 2013-2017. ONC Data Brief, no.45. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from http://searchhealthit.techtarget.com/blog/Health-IT-Pulse/Expansion-of-online-appointment-scheduling-could-lead-to-cost-savings
25 Patient Engagement: Digital self-scheduling set to explode. Retrieved from https://www.accenture.com/us-en/insight-patient-engagement-digital-self-scheduling-explode
26 Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
27 Kaiser Permanente 2014 Annual Report. Retrieved from http://share.kaiserpermanente.org/static/kp_annualreport_2014/
28 Timely access to scheduled appointments. Journal of the American Medical Informatics Association, 5(1), 104-111. Retrieved from https://healthy.kaiserpermanente.org/health/care/consumer/…/d5/L2dBISEvZ0FBIS9nQSEh/
29 Timely access to scheduled appointments. Journal of the American Medical Informatics Association, 5(1), 104-111. Retrieved from https://healthy.kaiserpermanente.org/health/care/consumer/…/d5/L2dBISEvZ0FBIS9nQSEh/
30 Henry J, Barker W, & Kachay L. (April 2019). Electronic capabilities for patient engagement among U.S. non-federal cute care hospitals: 2013-2017. ONC Data Brief, no.45. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from http://searchhealthit.techtarget.com/blog/Health-IT-Pulse/Expansion-of-online-appointment-scheduling-could-lead-to-cost-savings
31 Use Secure Electronic Messaging. Retrieved from https://www.healthit.gov/providers-professionals/achieve-meaningful-use/core-measures-2/use-secure-electronic-messaging
32 Kane, B., Sands, D.Z. (1998, January 1). Guidelines for the clinical use of electronic mail with patients. Retrieved from http://jamia.oxfordjournals.org/content/5/1/104
33 Kane, B., Sands, D.Z. (1998, January 1). Guidelines for the clinical use of electronic mail with patients. Retrieved from http://jamia.oxfordjournals.org/content/5/1/104
34 Fact Sheet: Using Secure Electronic Messaging to Support Patient and Family Engagement. Retrieved from https://www.healthit.gov/providers-professionals/implementation-resources/fact-sheet-using-secure-electronic-messaging
35 Meaningful Use Case Studies: Patient portal increases communication between patients and providers. (2011, Spring). Retrieved from https://www.healthit.gov/providers-professionals/blackstone-valley-community-health-care-case-study
36 Kane, B., Sands, D.Z. (1998, January 1). Guidelines for the clinical use of electronic mail with patients. Retrieved from http://jamia.oxfordjournals.org/content/5/1/104
37 Kane, B., Sands, D.Z. (1998, January 1). Guidelines for the clinical use of electronic mail with patients. Retrieved from http://jamia.oxfordjournals.org/content/5/1/104
38 Fact Sheet: Using Secure Electronic Messaging to Support Patient and Family Engagement. Retrieved from https://www.healthit.gov/providers-professionals/implementation-resources/fact-sheet-using-secure-electronic-messaging
39 Silvestre, A.-L.; Sue, V.M.; Allen, J.Y. (2009, March/April). If you build it, will they come? The Kaiser Permanente model of online health care. Health Affairs, 28(2), 334-344. doi 10.1377/hithaff.28.2.334. Retrieved from http://content.healthaffairs.org/content/28/2/334.full
40 Emont, S. (2011, May). Measuring the impact of patient portals: what the literature tells us. Retrieved from https://www.chcf.org/wp-content/uploads/2017/12/PDF-MeasuringImpactPatientPortals.pdf [PDF – 610KB]
41 Meaningful Use Case Studies: Patient portal benefits patient care and provider workflow. (2011, Winter). Retrieved from https://www.healthit.gov/case-study/patient-portal-benefits-patient-care-and-provider-workflow
42 Kessels, R.P.C. (2003, May). Patients’ memory for medical information. Journal of the Royal Society of Medicine, 96(5), 219-222. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC539473/
43 OpenNotes: Inviting patients to read their doctors’ visit notes. Retrieved from https://www.opennotes.org/research/inviting-patients-to-read-their-doctors-notes-patients-and-doctors-look-ahead-patient-and-physician-surveys/
44 OpenNotes: Inviting patients to read their doctors’ visit notes. Retrieved from https://www.opennotes.org/research/inviting-patients-to-read-their-doctors-notes-patients-and-doctors-look-ahead-patient-and-physician-surveys/
45 Siminerio, E.; Daniel, J.G. (2014, June 24). Patients play a vital role in improving the quality of information in their medical records. Retrieved from https://www.healthit.gov/buzz-blog/consumer/blue-button-helps-patients-improve-care-quality/
46 Delbanco, T.; Walker, J.; Bell, S.K.; Darer, J.D.; Elmore, J.G.; Farag, N.; Feldman, H.J.; Mejilla, R.; Ngo, L.; Ralston, J.D.; Ross, S.E.; Trivedi, N.; Vodicka, E.; Leveille, S.G. (2012, October 2). Annals of Internal Medicine, 157(7), 461-470. Retrieved from http://annals.org/article.aspx?articleid=1363511
47 What is OpenNotes? Retrieved from http://www.opennotes.org/about-opennotes/
48 Unitan, R. and Seidel, M. Sharing Visit Notes Online: Kaiser Permanente Northwest’s Big Bang Implementation of OpenNotes. (PowerPoint presentation, 2015, September 2). Retrieved from Kaiser Permanente Northwest.
49 Unitan, R. and Seidel, M. Sharing Visit Notes Online: Kaiser Permanente Northwest’s Big Bang Implementation of OpenNotes. (PowerPoint presentation, 2015, September 2). Retrieved from Kaiser Permanente Northwest.
50 Alpert J.M., Krist A.H., Aycock R.A., Kreps G.L. (2016, May 17). Applying Multiple Methods to Comprehensively Evaluate a Patient Portal’s Effectiveness to Convey Information to Patients. Retrieved from http://www.jmir.org
Chapter 3
51 Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
52 Wolff J.L., Darer J.D., Larsen K.L. Family Caregivers and Consumer Health Information Technology. J Gen Intern Med. 2016 Jan;31(1):117-21. doi: 10.1007/s11606-015-3494-0
53 Bourgeois, F.C.; Taylor, P.L.; Emans, J.; Nigrin, D.J.; Mandl, K.D. (2008, December). Whose personal control? Creating private, personally controlled health records for pediatric and adolescent patients. Journal of the American Medical Informatics Association, 15(6), 737–743. doi 10:1197/jamia.M2865. Retrieved from http://www.hl7.org/documentcenter/public_temp_7CA39230-1C23-BA17-0CBCDEB8D0B8876C/wg/pedsdata/Fabienne%20JAMIA%20paper%20(2).pdf [PDF – 78KB]
54 Bourgeois, F.C.; Nigrin, D.J.; Harper, M.B. (2015, May). Pediatrics perspectives. Preserving patient privacy and confidentiality in the era of personal health records. Journal of Adolescent Health, 135(5), e1125-e1127. Retrieved from http://pediatrics.aappublications.org/content/135/5/e1125
55 Jasik, C. (2005, February). UCSF goes live with teen patient portal. Retrieved from https://www.ucsfhealth.org/ucsfmychart/
56 Retrieved from https://www.coloradohealth.org/portal-support-non-english-speaking-patients
Chapter 4
57 Henry J, Barker W, & Kachay L. (April 2019). Electronic capabilities for patient engagement among U.S. non-federal cute care hospitals: 2013-2017. ONC Data Brief, no.45. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from http://searchhealthit.techtarget.com/blog/Health-IT-Pulse/Expansion-of-online-appointment-scheduling-could-lead-to-cost-savings
58Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
59 HIM Body of Knowledge™. Retrieved from http://bok.ahima.org/
60 45 Code of Federal Regulations 164.502(g). Cornell University Legal Information Institute. Uses and disclosures of protected health information: general rules. Retrieved from https://www.law.cornell.edu/cfr/text/45/164.502
61 Wolff J.L., Darer J.D., Larsen K.L. Family Caregivers and Consumer Health Information Technology. J Gen Intern Med. 2016 Jan;31(1):117-21. doi: 10.1007/s11606-015-3494-0
62 45 Code of Federal Regulations 164.510(b). Cornell University Legal Information Institute. Uses and disclosures requiring an opportunity for the individual to agree or to object. Retrieved from https://www.law.cornell.edu/cfr/text/45/164.510
63 45 Code of Federal Regulations 164.510(b). Cornell University Legal Information Institute. Uses and disclosures requiring an opportunity for the individual to agree or to object. Retrieved from https://www.law.cornell.edu/cfr/text/45/164.510
64 Wolff J.L., Kim V.S., Mintz S., Stametz R., Griffin J.M. An environmental scan of shared access to patient portals. J Am Med Inform Assoc. 2017 Aug 25. doi: 10.1093/jamia/ocx088
65 Wolff J.L., Darer J.D., Larsen K.L. Family Caregivers and Consumer Health Information Technology. J Gen Intern Med. 2016 Jan;31(1):117-21. doi: 10.1007/s11606-015-3494-0
66 Wolff J.L., Kim V.S., Mintz S., Stametz R., Griffin J.M. An environmental scan of shared access to patient portals. J Am Med Inform Assoc. 2017 Aug 25. doi: 10.1093/jamia/ocx088
67 Retrieved from http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/development-of-a-tethered-personal-health-record-framework-for-early-end-of-life-discussions
68 Retrieved from https://patientengagementhit.com/news/how-patient-portals-can-improve-advance-care-planning-talks
Chapter 5
69 Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
70 Patel V & Johnson C. (February 2018). Consumers' use of online medical records and devices for health needs. ONC Data Brief, no.40. Office of the National Coordinator for Health Information Technology: Washington DC. Retrieved from https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf [PDF - 1.7 MB]
71 Patient-Generated Health Data. (2015, September 30). Retrieved from https://www.healthit.gov/policy-researchers-implementers/patient-generated-health-data
72 National Learning Consortium. (2014, March). Patient-Generated Health Data Fact Sheet. Retrieved from https://www.healthit.gov/sites/default/files/patient_generated_data_factsheet.pdf [PDF – 1.6MB]
73 Centers for Medicare & Medicaid Services. (2016, April). Readmissions Reduction Program. Retrieved from https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html
74 The Digital Consumer: How Patient Generated Health Data and Health IT Can Help Improve Care. Retrieved from https://www.healthit.gov/buzz-blog/consumer/digital-consumer-patient-generated-health-data-improve-care/
75 National Learning Consortium. (2014, March). Patient-Generated Health Data Fact Sheet. Retrieved from https://www.healthit.gov/sites/default/files/patient_generated_data_factsheet.pdf [PDF – 1.6MB]
76 Lavallee, D.; Chenok, K.; Love, R.; Petersen, C.; Holve, E.; Segal, C.; and Franklin, P. (2016). Incorporating Patient-Reported Outcomes Into Health Care to Engage Patients and Enhance Care. Health Affairs, 35(4), doi: 10.1377/hlthaff.2015.1362. Retrieved from http://content.healthaffairs.org/content/35/4/575.full?ijkey=6C1y7.jaIT7qU&keytype=ref&siteid=healthaff#aff-1
77 National Learning Consortium. (2014, March). Patient-Generated Health Data Fact Sheet. Retrieved from https://www.healthit.gov/sites/default/files/patient_generated_data_factsheet.pdf [PDF – 1.6MB]
78 Ochsner Health System first epic client to fully integrate with Apple HealthKit Call-out box: Retrieved from https://news.ochsner.org/news-releases/ochsner-health-system-first-epic-client-to-fully-integrate-with-apple-healt
79 Develop health and fitness apps that work together. Retrieved from https://developer.apple.com/healthkit/
80 Nield, D. (2016, April 27). 25 essential fitness apps that work with Apple Health: updated Apple Health compatible apps and devices for complete health tracking. Retrieved from http://www.wareable.com/sport/apps-that-work-with-apple-health-kit-compatible
81 Ochsner Health System first epic client to fully integrate with Apple HealthKit Call-out box: Retrieved from https://news.ochsner.org/news-releases/ochsner-health-system-first-epic-client-to-fully-integrate-with-apple-healt
82 Ochsner Health system first in nation to manage chronic diseases with Apple Watch. (2014). Retrieved from https://news.ochsner.org/news-releases/ochsner-health-system-first-in-nation-to-manage-chronic-diseases-with-apple
83 Ochsner Health System continues to transform healthcare with “Optimal Hospital”: innovative program uses Apple Watch, iPad and iPhone to introduce a new model for care as a way to manage efficiencies in hospital care. (2016, February 24). Retrieved from https://news.ochsner.org/news-releases/ochsner-health-system-continues-to-transform-healthcare-with-optimal-hospit
84 Access to MyCarolinas is easy. (2016) Retrieved from https://my.carolinashealthcare.org/login.aspx?ReturnUrl=%2fdefault.aspx
85 Carolinas HealthCare System. Retrieved from https://www.healthit.gov/sites/default/files/carolinas_healthcare_commitment.pdf [PDF – 153KB]
86 Broderick, A. (2013, January). Case Studies in Telehealth Adoption. Partners HealthCare: connecting heart failure patients to providers through remote monitoring. Commonwealth Fund Publication 1656, 3. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/case-study/2013/jan/1656_broderick_telehealth_adoption_partners_case_study.pdf [PDF – 610KB]
87 Remote monitoring program for heart failure patients significantly lowers hospital admissions: less intensive remote monitoring follow-up may improve long-term outcomes. (2015, May 13). Retrieved from http://connectedhealth.partners.org/news-and-events/media-center/announcements/heart-failure-remote-monitoring-program-significantly-lowers-hospital-admissions.aspx
88 Agboola, S.; Jethwani, K.; Khateeb, K.; Moore, S.; Kvedar, J. (2015). Heart failure remote monitoring: Evidence from the retrospective evaluation of a real-world remote monitoring program. Journal of Medical Internet Research, 17(4), e101. doi:10.2196/jmir.4417. Retrieved from http://www.jmir.org/2015/4/e101
89 Broderick, A. (2013, January). Case Studies in Telehealth Adoption. Partners HealthCare: connecting heart failure patients to providers through remote monitoring. Commonwealth Fund Publication 1656, 3. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/case-study/2013/jan/1656_broderick_telehealth_adoption_partners_case_study.pdf [PDF – 610KB]
90 Agboola, S.; Jethwani, K.; Khateeb, K.; Moore, S.; Kvedar, J. (2015). Heart failure remote monitoring: Evidence from the retrospective evaluation of a real-world remote monitoring program. Journal of Medical Internet Research, 17(4), e101. doi:10.2196/jmir.4417. Retrieved from http://www.jmir.org/2015/4/e101
91 Remote monitoring program for heart failure patients significantly lowers hospital admissions: less intensive remote monitoring follow-up may improve long-term outcomes. (2015, May 13). Retrieved from http://connectedhealth.partners.org/news-and-events/media-center/announcements/heart-failure-remote-monitoring-program-significantly-lowers-hospital-admissions.aspx
92 Broderick, A. (2013, January). Case Studies in Telehealth Adoption. Partners HealthCare: connecting heart failure patients to providers through remote monitoring. Commonwealth Fund Publication 1656, 3. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/case-study/2013/jan/1656_broderick_telehealth_adoption_partners_case_study.pdf [PDF – 610KB]
93 Broderick, A. (2013, January). Case Studies in Telehealth Adoption. Partners HealthCare: connecting heart failure patients to providers through remote monitoring. Commonwealth Fund Publication 1656, 3. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/case-study/2013/jan/1656_broderick_telehealth_adoption_partners_case_study.pdf [PDF – 610KB]
94 Broderick, A. (2013, January). Case Studies in Telehealth Adoption. Partners HealthCare: connecting heart failure patients to providers through remote monitoring. Commonwealth Fund Publication 1656, 3. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/case-study/2013/jan/1656_broderick_telehealth_adoption_partners_case_study.pdf [PDF – 610KB]
95 Orlando, L.A.; Hauser, E.R.; Christianson, C.; Powell, K.P.; Buchanan, A.H.; Chesnut, B.; Agbaje, A.B.; Henrich, V.C.; Ginsburg, G. (2011, October 11). Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Services Research 11, 264. doi: 10.1186/1472-6963-11-264. Retrieved from http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-264
96 Orlando, L.A.; Hauser, E.R.; Christianson, C.; Powell, K.P.; Buchanan, A.H.; Chesnut, B.; Agbaje, A.B.; Henrich, V.C.; Ginsburg, G. (2011, October 11). Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Services Research 11, 264. doi: 10.1186/1472-6963-11-264. Retrieved from http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-264
97 Orlando, L.A.; Hauser, E.R.; Christianson, C.; Powell, K.P.; Buchanan, A.H.; Chesnut, B.; Agbaje, A.B.; Henrich, V.C.; Ginsburg, G. (2011, October 11). Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Services Research 11, 264. doi: 10.1186/1472-6963-11-264. Retrieved from http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-264
98 Wu, R.R.; Himmel, T.L.; Buchanan, A.H.; Powell, K.P.; Hauser, E.R.; Ginsburg, G.S.; Henrich, V.C.; Orlando, L.A. (2014, February 13). Quality of family history collection with use of a patient facing family history assessment tool. doi: 10.1186/1471-2296-15-31. Retrieved from https://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-15-31
99 Orlando, L.A.; Hauser, E.R.; Christianson, C.; Powell, K.P.; Buchanan, A.H.; Chesnut, B.; Agbaje, A.B.; Henrich, V.C.; Ginsburg, G. (2011, October 11). Protocol for implementation of family health history collection and decision support into primary care using a computerized family health history system. BMC Health Services Research 11, 264. doi: 10.1186/1472-6963-11-264. Retrieved from http://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-264
100 Fast Healthcare Interoperability Resources overview. Retrieved from https://www.hl7.org/fhir/overview.html
101 Time to focus on your family tree. (2015, December 15). Call-out box: Retrieved from https://today.duke.edu/2015/12/metree
Chapter 6
102 Pew Research Center (February 2018). Mobile Fact Sheet. Retrieved from http://www.pewinternet.org/fact-sheet/mobile/
103 Comstock, Jonah (2013, October 24). Digitas Health: Patients whose doctors use apps use more apps themselves. MobiHealthNews. Retrieved from https://www.mobihealthnews.com/26642/digitas-patients-whose-doctors-use-apps-use-more-apps-themselves
104 Groshek, M. R., Oldenburg, J., Sarasohn-Kahn, J., & Sitler, B. (2015, February 20). mHealth App Essentials: Patient Engagement, Considerations, and Implementation. Retrieved from https://www.himss.org/mhealth-app-essentials-patient-engagement-considerations-and-implementation
105 Byambasuren, O., Sanders, S., Beller, E., & Glasziou, P., (2018, May 9). Prescribable mHealth apps identified from an overview of systematic reviews. npj Digital Medicine. Retrieved from https://www.nature.com/articles/s41746-018-0021-9
106 Boudreaux, E. D., Waring, M. E., Hayes, R. B., Sadasivan, R. S., Mullen, S., & Pagoto, S. (2014, September 24). Evaluating and selecting mobile health apps: strategies for healthcare providers and healthcare organizations. Translational Behavioral Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286553/
107 Bell, S.K., Mejilla, R., Anselmo, M., et al. When doctors share visit notes with patients: a study of patient and doctor perceptions of documentation errors, safety opportunities and the patient–doctor relationship. BMJ Qual Saf 2017;26:262-270. Retrieved from: https://qualitysafety.bmj.com/content/26/4/262.abstract
108 Asan, O., Tyszka, J., Crotty, B. (2018, 1 July). The electronic health record as a patient engagement tool: mirroring clinicians’ screen to create a shared mental model. JAMIA Open, Volume 1, Issue 1, Pages 42–48. Retrieved from: https://doi.org/10.1093/jamiaopen/ooy006
109 Asan, O., Tyszka, J., Crotty, B. (2018, 1 July). The electronic health record as a patient engagement tool: mirroring clinicians’ screen to create a shared mental model. JAMIA Open, Volume 1, Issue 1, Pages 42–48. Retrieved from: https://doi.org/10.1093/jamiaopen/ooy006
110 The Office of the National Coordinator for Health Information Technology. (2017, September 28). Telemedicine and telehealth. Retrieved from: https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth
111 Abrams, K., Burrill, S., & Elsner, N. (2018, July 18). What can health systems do to encourage physicans to embrace virtual care? Deloitte Insights. Retrieved from: https://www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-health-consumer-and-physician-surveys.html
112 Abrams, K., Burrill, S., & Elsner, N. (2018, July 18). What can health systems do to encourage physicans to embrace virtual care? Deloitte Insights. Retrieved from: https://www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-health-consumer-and-physician-surveys.html
113 Findlay, S. (2018, May 6). Virtual doctor visits are getting more popular, but questions remain about who pays. Washington Post. Retrieved from: https://www.washingtonpost.com/national/health-science/virtual-doctor-visits-are-getting-more-popular-but-questions-remain-about-who-pays/2018/05/04/cbe262f6-4c85-11e8-b725-92c89fe3ca4c_story.html?utm_term=.77c7cee0782b
114 Findlay, S. (2018, May 6). Virtual doctor visits are getting more popular, but questions remain about who pays. Washington Post. Retrieved from: https://www.washingtonpost.com/national/health-science/virtual-doctor-visits-are-getting-more-popular-but-questions-remain-about-who-pays/2018/05/04/cbe262f6-4c85-11e8-b725-92c89fe3ca4c_story.html?utm_term=.77c7cee0782b
115 Major, J. (2016, November 17). Using Telemediquette to Make Your Telemedicine Encounters Effective. The Arizona Telemedicine Program Blog. Retrieved from: https://telemedicine.arizona.edu/blog/using-telemediquette-make-your-telemedicine-encounters-effective